GOLD 1
Nothing is impossible- the word itself says “I’m Possible”
NCLEX TIPS
- Do not read into the question– never assume anything that has not been specifically mentioned (in the question) and do not add extra meaning or history to the question—do not make up a story to validate choosing an answer
- NCLEX land is set at Utopia General Hospital- you have all the time, all the resources, and all the staff you need!
- Least invasive to most invasive – least restrictive to most restrictive (restraints are rarely a good choice)
- Avoid using absolutes– always, never, must, etc.
- Assess the client first before implementing a treatment or action—if there’s a choice that pertains to assessment of the patient—it is usually the answer – assess unless in distress
- Priority goes to assessments and answers that deal with the patient (patient-focused) directly and not with machines/monitors/equipment (unless the question is specifically asking about them)
- Ex: Auscultate fetal heart rate before checking the monitor
- If it is the FIRST time doing something for or with the patient (such as vital signs upon admission to the floor/unit, or when a transfer is involved), the NURSE must complete the assessment- including vital signs
- If patient is an adult, answers with family options can be ruled out (unless patient is not competent to make own decisions)
- In emergency situations (mass casualty), patients with greater chance to live are treated first
- If you are asked about the FIRST action you would take in a prioritization/discrimination question think: “If I can only do one action, and then I must go home, what will the outcome be?”
- Therapeutic communication- reflect feelings and provide correct information
- Do not ask “why” questions (or yes/no) and do not say “I understand”
- An answer that delays care or treatment is usually wrong (Ex: reassess in 15 minutes, monitor the patient for a continuation of symptoms)
- When determining interventions to enhance a client’s wellness, consider options that promote healthy nutrition, regular exercise, proper weight maintenance, proper rest, and avoidance of harmful chemicals (nicotine) and risk-taking behaviors (not wearing a seat belt)
- If two of the answer choices are the exact opposite, one is probably the answer (ie. bradycardia, tachycardia)
- If two or three answers are similar, none are correct (*be careful—sometimes answers may seem similar but in fact are saying something different)
- Always look for the UMBRELLA option—one that is a broad universal statement and usually contains the concepts of the other options with it—often the correct answer
- If you have never heard of an answer—do not eliminate it—work around it…if you can safely eliminate all other answers, that is your answer—if you are down to two answers and you know one answer is right, go with what you know
- Prioritize actual problems over potential problems
- DO NOT leave the patient – think safety
- DO NOT “do nothing”- you always have to do something
- If the question is about endorsement—always report anything new or different to the next shift
- Only select “document” if the assessment is normal
- Put patients with the same or similar diagnoses in the same room-clean vs. dirty patients
- Never increase a patient’s fluids to “catch up”
- Answer SATA questions as true or false for each answer option
- Rephrase the question in your own words—this ensures you understand what the question is asking—if you cannot rephrase the question, you do not know what the topic is
- If you cannot determine the topic of the question, read all answer choices to help you understand the problem (look for patterns)
- Try not to determine the answer before reading the answer choices—NCLEX uses traps and answers that scream “pick me” but are wrong
- More often than not, pain will not be your answer — pain is considered psychosocial—exception to this rule are signs and symptoms of compartment syndrome
- Try to focus on the here and now as much as possible
- With positioning questions- you are trying to prevent or promote something—evaluate the outcome of each option
- When the question asks what is ESSENTIAL—think SAFETY
- If you do not know what a word means, try to break it down using medical terminology
- Ex: Rhabdomyosarcoma – muscle (myo), tumor (sarcoma) →
tumor of the muscle tissue
-
- Same idea applies to medications- use suffixes and prefixes to recognize classifications
- Make an educated guess—if you can’t make the best answer for a question after carefully reading it, choose the answer with the most information
- When in doubt, SAFETY
“Keep them breathing, keep them safe”
Prioritization Techniques
- Prioritize systemic vs. local (life before limb)
- Prioritize acute before chronic
- Prioritize actual before potential future problems
- Prioritize according to Maslow’s- physiological needs before psychosocial (acute safety can take priority- ATI)
- Recognize and respond to trends vs. transient findings (recognizing a gradual deterioration)
- Recognize signs of emergencies and complications vs. “expected client findings”
- Apply clinical knowledge to procedural standards to determine the priority action- recognizing that the timing of administration of antidiabetic and antimicrobial medications is more important than administration of some other medications
How to tackle- WHO DO YOU SEE FIRST- questions:
- Who is your most stable patient? ELIMINATE ANSWER
- Who is your most stable patient (of the 3 remaining)? ELIMINATE ANSWER
- Who is your most unstable patient (of the 2 remaining)? Airway? Breathing? Circulation? SELECT ANSWER
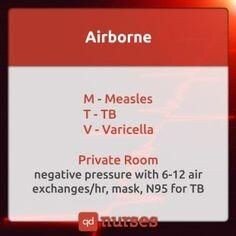
Transmission-Based Precautions AIRBORNE
MTV
M- measles T- TB
V- Varicella (chicken pox), varicella zoster (disseminated shingles)
*Private room– negative pressure with 6-12 air exchanges/hr, mask, N95
Chicken pox can be rapidly transmitted to other clients—should be isolated quickly and placed in negative pressure room
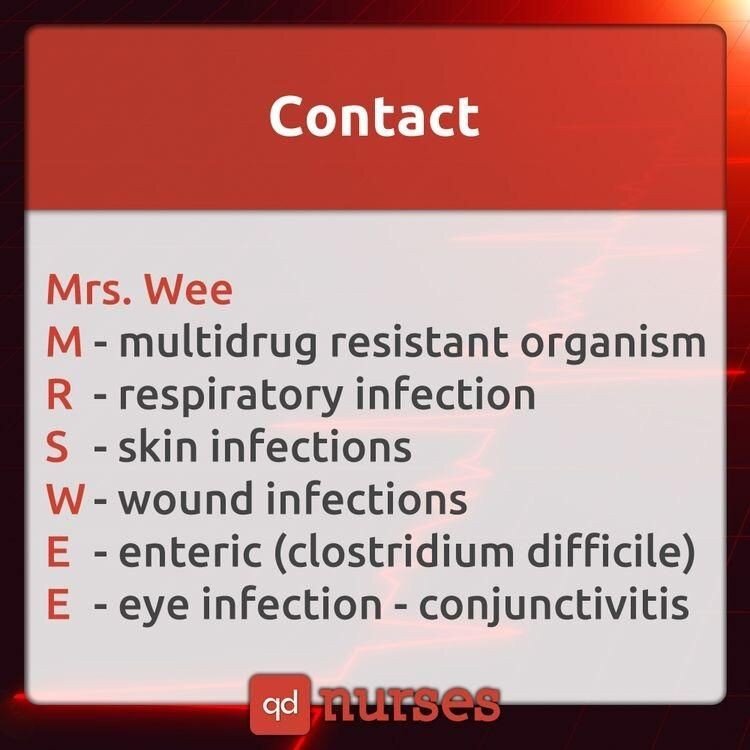
CONTACT
MRS. WEE
M- multidrug resistant organism (MRSA) R- respiratory infection
S- skin infections (localized herpes zoster) W- wound infections
E- enteric infection → clostridium difficile E- eye infection → conjunctivitis
(Also, Hep A)
*A nurse with localized herpes zoster CAN care for patients as long as the patients are NOT immunocompromised and the lesions are covered!
DROPLET
SPIDERMAN
S- sepsis
S- scarlet fever
S- streptococcal pharyngitis P- parvovirus B19
P- pneumonia (pneumonic plague) P- pertussis
I- influenza
D- diphtheria (pharyngeal)
E- epiglottitis R- rubella
R- respiratory syncytial virus (RSV) M- mumps
M- meningococcal (infectious meningitis) M- mycoplasma or meningeal pneumonia An- adenovirus
*Private room or cohort, mask (door open, 3ft distance)
Current CDC evidence-based guidelines indicate that droplet precautions for clients with meningococcal meningitis can be discontinued when the client has received antibiotic therapy for 24 hours!

Current CDC guidelines indicate that rapid implementation of standard, contact, and airborne precautions are needed for any client suspected of having SARS—in order to protect other clients and healthcare workers
Skin Infections
VCHIPS
V- varicella zoster
C- cutaneous diphtheria H- herpes simplex
- impetigo
P- pediculosis S- scabies
Impetigo– caused by Staph and Strep, untreated can cause acute glomerulonephritis (periorbital edema—indicates poststreptococcal glomerulonephritis)
Order of PPE Application
-
- Gown
- Mask
- Goggles/face shield
- Gloves
Order of PPE Removal
-
- Gloves
- Goggles/face shield
- Gown
- Mask
Because the hands of health care workers are the most common means of transmission of infection from one client to another, the most effective method of preventing the spread of infection is to make supplies for hand hygiene readily available for staff to use.
Because the respiratory manifestations associated with the avian influenza are potentially life threatening, the nurse’s initial action should be to start oxygen therapy!
- S/S: SOB, diarrhea, abdominal pain, epistaxis
- Institute airborne and contact precautions
According to the CDC, catheter associated UTIs are the most common health care-acquired infection in the US—primary CDC recommendations include avoiding the use of indwelling catheters and the removal of catheters as soon as possible!
Individuals who have contact with infants should be immunized against pertussis in order to avoid infection and to prevent transmission to the infant!
The ventilator bundle developed by the Institute for Healthcare Improvement includes recommendations for continuous elevation of the head of the bed (30 to 45 degrees), daily assessment for extubation readiness, and daily oral care with chlorhexidine solution.
Chlorhexidine is more effective than the other options at reducing the risk for central-line associated bloodstream infections (CLABSIs)
No pee, no K (do not give potassium without adequate urine output)
ElVate Veins, dAngle Arteries for better perfusion
*IV push should be given over 2 minutes*
CONVERSIONS
| 1 oz | 30 mL |
| 1 cup | 8 oz |
| 1 kg | 2.2 lbs |
| 1 lb | 16 oz |
| 1 gr (grain) | 60 mg |
| *Convert C to F: C + 40 multiply by 9/5 and subtract 40
*Convert F to C: F + 40 multiply by 5/9 and subtract 40 |
|
Positioning _
Asthma
- Orthopneic position where patient is sitting up and bent forward with arms support on a table or chair arms
Air Embolism- (S/S: chest pain, difficulty breathing, tachycardia, pale/cyanotic, sense of impending doom)
- Turn patient to LEFT side and LOWER head of bed
Pulmonary Embolism- (S/S: chest pain, difficulty breathing, tachycardia, pale/cyanotic, sense of impending doom)
- Elevate HOB
Women in Labor with non-reassuring FHR- (S/S: late decels, decreased variability, fetal bradycardia, etc.)
- Turn mother on LEFT side (and give O2, stop Pitocin, increase IV fluids)
Tube Feeding w/ Decreased LOC
- Head of bead ELEVATED (to prevent aspiration) and position patient on
RIGHT side (promotes gastric emptying)
Postural Drainage
- Lung segment to be drained should be in the uppermost position to allow gravity to work
During Epidural/Lumbar Puncture
- Side-lying (“C” curved spine)- lateral recumbent/fetal position
Post Lumbar Puncture (LP) – (and also oil-based myelogram)
- Patient lies in flat supine (to prevent CSF leak and headache) for 2-3 hours
- Sterile dressing applied
- Frequent neuro checks
Thoracentesis
- Position patient with arms on pillow over bed table or lying on side
NO MORE THAN 1000cc at one time
- Post- check blood pressure, auscultate bilateral breath sounds, check for leakage, sterile dressing
Patient with Heat Stroke
- Lie flat with legs elevated
Hemorrhagic Stroke
- HOB elevated 30 degrees to reduce ICP and facilitate venous drainage
Ischemic Stroke
- HOB flat (supine)
During Continuous Bladder Irrigation (CBI)– catheter is taped to thigh
- Leg should remain straight to prevent pulling on catheter
Post Myringotomy– surgical incision in eardrum to relieve pressure and drain fluid (tubes)
- Position on side of affected ear after surgery (allows drainage of secretions)
Post Cataract Surgery
- Patient will sleep on unaffected side with night shield for 1-4 weeks (adequate vision may not return for 24 hours)
- Pain that is not relieved by prescription pain medication may signal hemorrhage, infection or increased ocular pressure
Infant with Spina Bifida
- Position prone (on abdomen) to prevent sac from rupturing
Buck’s Traction (skin traction)
- Elevate foot of bed for counter-traction
Post Total Hip Replacement
- DON’T sleep on affected/operative side
- DON’T flex hip more than 45-60 degrees
- DON’T elevate HOB more than 45 degrees
- Maintain hip abduction by separating thighs with a pillow
NO adduction or internal rotation
Prolapsed Cord
- Knee-chest or Trendelenburg (goal is to prevent pressure on cord)

Vena Cava Syndrome (pregnant women)
- Position woman on her left side (relieves pressure off vena cava from fetus)—knees flexed (blood return)
o Mother may present with hypotension
Infant with Cleft Lip
- Position on back or in an infant seat to prevent trauma to suture line
- While feeding, hold in upright position
Infant with Cleft Palate
- Prone
Pancreatitis
- Patients should lie in fetal position
- Maintain NPO status (to rest the gut)—patient may also have PICC line inserted for TPN/lipids
To Prevent Dumping Syndrome
- Eat in reclining position
- Lie down after meals for 20-30min
- Restrict fluids during meals, low carbohydrate, low fiber, high fat and protein
- *GOAL: decrease gastric motility
Enema Administration
- Position patient in left-side lying (Sim’s position) with knees flexed
Above Knee Amputation
- Elevate for first 24 hours on pillow
- Position prone daily to provide for hip extension
- Do not keep leg elevated beyond 24 hours—causes hip flexion which can lead to contractures
- Rewrap 3x day (elastic bandages)
Below Knee Amputation
- Foot of bed elevated for first 24 hours
- Position prone daily to provide for hip extension
- Do not keep leg elevated beyond 24 hours—causes hip flexion which can lead to contractures
*Activity helps reduce the frequency and degree of phantom pain Detached Retina
- Area of detachment should be in the dependent position (head in
downward direction, lying on unaffected side)
After Supratentorial Surgery (suture behind hairline)
- Elevate HOB 30-45 degrees
After Intratentorial Surgery (incision at nape of neck)
- Position patient flat and lateral on either side
During Internal Radiation
- On bed rest while implant is in place
*(Common NCLEX TOPIC)
Autonomic Dysreflexia/Hyperreflexia (S/S: pounding H/A, profuse sweating, nasal congestion, goose flesh, bradycardia, HTN)
- Place patient in sitting position- HIGH FOWLER’S (elevate HOB- FIRST ACTION)—decreases venous return
- Check for kinks in foley catheter tubing
Spinal Cord Injury
- Immobilize on spine board
- Head in neutral position
- Immobilize with padded C-collar
- Maintain traction and alignment of head manually
- Log roll client and do not allow to twist or bend
Shock
- Bed rest with extremities elevated 20 degrees, knees straight, head slightly elevated (modified Trendelenburg)
Head Injury
- Elevate HOB 30 degrees to decrease ICP
Peritoneal Dialysis when Outflow is Inadequate
- Turn patient from side to side BEFORE checking for kinks in tubing (according to Kaplan)
Nasogastric Tube
- Elevate HOB 30 degrees to prevent aspiration
- Maintain elevation for continuous feeding or 1 hour after intermittent feedings
Cardiac Catheterization
- Keep site extended (usually involves femoral artery)
Post-thyroidectomy
- Semi-Fowler’s position, prevent neck flexion/hyperextension (support head, neck and shoulders)
- Trach at bedside
- Monitor respiratory status every hour
Post-Bronchoscopy
- Semi Fowler’s
- Check V/S q15 min until stable
- Assess for respiratory difficulty (stridor, dyspnea resulting from laryngeal edema or laryngospasm)
Epistaxis
- Upright and lean forward (prevent blood from entering the stomach and to avoid aspiration)
Pelvic Exam
- Lithotomy position
Rectal Exam
- Knee-chest position, Sim’s, or dorsal recumbent
Post-Liver Biopsy
- Place patient on right side over a pillow to prevent bleeding (liver is very vascular)
- No heavy lifting for 1 week’
Paracentesis
- Semi-Fowler’s or upright on edge of bed
- Void prior- prevent puncture of bladder
- Post- V/S (BP), report elevated temp, observe for signs of hypovolemia
Pneumonia
- Lay on affected side to splint and reduce pain
- Trying to reduce congestion: the sick lung goes up
Post-Appendectomy
- Position on right side with legs flexed
GERD
- Lay on left side with HOB elevated 30 degrees (increases sphincter pressure)
Postural Drainage
- Head in dependent position
Post-Radical Mastectomy
- Position in Semi-Fowler’s with arm (affected side) elevated – if left mastectomy, elevate left arm, if right mastectomy, elevate right arm!
o This facilitates removal of fluid through gravity and enhances circulation
Think positively and you can achieve great things!
Prior to liver biopsy it is important to check lab results for PT time (vascular organ)
Liver biopsy– (prior) administer Vitamin K, NPO at midnight, teach patient that he will be asked to hold breath for 5-10 sec, supine position with upper arms elevated
Morphine is contraindicated in pancreatitis—it causes spasm of the Sphincter of Oddi—Demerol is the pain medication of choice!
*After pain relief, it is important to cough and deep breathe in pancreatitis—because fluid is pushing up in the diaphragm
*With chronic pancreatitis, pancreatic enzymes are given with meals
Diabetes Mellitus- pancreatic disorder resulting in insufficient or lack of insulin production leading to elevated blood sugar
- Type I (insulin dependent)- immune disorder, body attacks insulin producing beta cells with resulting Ketosis (result of ketones in blood due to gluconeogenesis from fat)
- Excessive thirst and weight loss are characteristic of T1DM
- Type II (insulin resistant)- beta cells do not produce enough insulin or body becomes resistant
NCLEX Points
-
- Assessment
- 3 P’s
- Polyuria (excessive urination), polydipsia (extreme thirst), polyphagia (excessive hunger)
- Elevated blood sugar
- Blurred vision
- Elevated HbA1C
- Poor wound healing
- Neuropathy
- Inadequate circulation
- End organ damage is a major concern due to damage to vessels
- Coronary artery disease
- HTN, cerebrovascular disease
- Retinopathy
- Coronary artery disease
- 3 P’s
- Assessment
Therapeutic Management
-
-
- Insulin
- Required for Type I and for Type II when diet and exercise do not control blood sugar
- Assess for and teach the patient regarding peak action time for various insulins
- Only administer short acting insulins IV
- Do not use vial that appears cloudy (NPH is the exception)
- Patient should monitor blood sugar before, during, and after exercise
- Patient should use protective footwear to prevent injury
- Infections and wounds should receive meticulous care
- Foot Care (inspect daily)
- Feet should be kept dry
- Footwear should always be worn (cotton socks are recommended as well as properly fitted shoes)
- Should not wear tight fitting socks
- Sick Day – when patients with DM become ill, glucose levels become elevated
- Continue to check blood sugars and do not withhold insulin
- Monitor for ketones in urine
- 15 Rule
- If blood sugar is low, administer 15g carbohydrates (5 lifesavers, 6 oz juice)- recheck in 15 minutes
- Complications
- Lipoatrophy
- Loss of subq fat at injection site (alternate injection sites)
- Lipohypertrophy
- Fatty mass at injection site
- Dawn phenomenon
- Reduced insulin sensitivity between 5-8AM
- Evening administration may help
- Adjust evening diet, bedtime snack, insulin dose, and exercise to prevent early morning hyperglycemia – adjust do not eliminate (usually intermediate acting insulin is used)
- Somogyi phenomenon
- Night time hypoglycemia results in rebound hyperglycemia in the morning hours
- Lipoatrophy
- Insulin
-
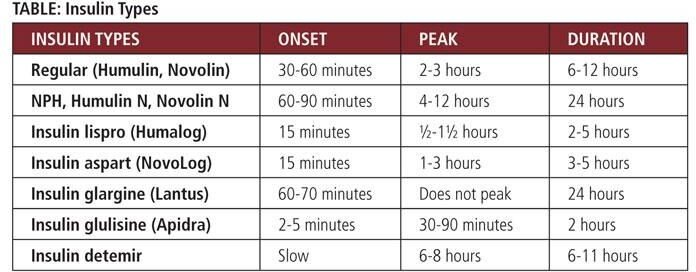
Rapid-acting insulin should only be given if food is available and patient is ready to eat
Repaglinide is a meglitinide analog drug—short-acting agents used to prevent postmeal blood glucose elevation—should be given within 1 to 30 minutes before meals and cause hypoglycemia shortly after dosing when a meal is denied or omitted

Drawing up regular insulin and NPH together
Cloudy (air into NPH) Clear (air into regular) Clear (draw up regular) Cloudy (draw up NPH) Or
RN- regular before NPH
Hypoglycemia requires urgent treatment
- Signs and Symptoms
- Hunger
- Irritability
- Weakness
- Headache
- BG < 60
- Consume 10 to 15g of carbohydrate (15-Rule)
- Glucose should be retested in 15 min
- Patient should eat a small snack of carbohydrate and protein if the next meal is more than an hour away
- Repeat carbohydrate treatment if symptoms do not resolve
Alcohol has the potential for causing alcohol-induced hypoglycemia—it is important to know when the patient drinks alcohol and to teach the patient to ingest it shortly after meals to prevent this complication
Guidelines for exercise are based on blood glucose and urine ketone level—patients should test blood glucose before, during, and after exercise to be sure that it is safe.
- When ketones are present the patient should not exercise because they indicate that current insulin levels are not adequate
Diabetic Ketoacidosis (DKA)– body is breaking down fat instead of sugar for energy—fats leave ketones (acids) that cause pH to decrease
*DKA is rare in DM Type 2 because there is enough insulin to prevent breakdown of fats
- Serum acetone and serum ketones increase in DKA
- As you treat the acidosis and dehydration expect the potassium to drop rapidly → be ready with potassium replacement
- Fluids are the most important intervention for DKA and HHNS
- NS or LR
- Second voided urine is the most accurate when testing for ketones and
glucose
- Bringing the glucose down too much too quickly can result in increased ICP due to water being pulled into the CSF
- Urine ketone testing should be done whenever the patient’s blood glucose is greater than 240
Hyperosmolar Hyperglycemic Nonketotic Syndrome (HHNS)
- Potassium is low due to diuresis
- Fluids are the most important intervention
- No acidosis and no ketosis
- Weight loss is a symptom
- Often occurs in older adults with T2 Diabetes
- Risk Factors
- Diuretics
- Inadequate fluid intake (dehydration)
HbA1c- assesses how well blood sugar has been managed over 3 month period- 4 to 6% is good; 8% or greater indicates poor control
- 7% is ideal for a diabetic
Usually hold insulin prior to surgery and monitor blood glucose
To Remember Blood Sugar
Hot and dry, sugar high (hyperglycemia)
Cold and clammy, need some candy (hypoglycemia)
Laparoscopy- CO2 is used to enhance visual—general anesthesia, foley catheter
Post-op: EARLY AMBULATION to mobilize CO2
Myasthenia Gravis- decrease in receptor sites for acetylcholine- because the smallest concentration of ACTH receptors are cranial nerves, expect fatigue and weakness in eye, mastication/chewing, and pharyngeal muscles
Sometimes the first sign is that the patient can’t brush their hair
*Not enough receptor sites for Acetylcholine to bind to for activation—leading to muscle weakness
*Worsens with exercise and improves with rest
- Diagnosis is made via Tensilon test- improvement in muscle weakness (short period of time) indicates a positive reaction
- Avoid alcohol, crowded places, try to reduce stress, avoid heat (sauna, hot tub, sunbathing), spread activities throughout the day, thicken liquids
Myasthenic Crisis: often follows some type of infection—client is at risk for inadequate respiratory function
- S/S: elevated temperature, tachycardia, HTN, incontinent of urine and stool
Cholinergic Crisis: caused by excessive medication, stop med→ Tensilon will make it worse
Head injury Medication
- Manntiol (osmotic diuretic)—crystallizes at room temperature so
ALWAYS use a filter needle!
Endocrine System
| Hormone | Gland |
| Growth Hormone (GH) | Anterior Pituitary |
| ADH | Posterior Pituitary |
| T3, T4 | Thyroid |
| PTH | Parathyroid |
| Glucocorticoids: cortisol | Adrenal gland |
| Insulin | Pancreas |
*Parathyroid gland relies on the presence of Vitamin D to work
Palpate the thyroid gently- can cause thyroid storm in a patient with hyperthyroidism
After removal of pituitary gland- watch for hypocortisolism and temporary Diabetes Insipidus
Myxedema/Hypothyroidism- hyposecretion of thyroid hormone (TH) resulting in decreased metabolic rate (slowed physical and mental function)
- Myxedema coma- life threatening state of decreased thyroid production—coma result of acute illness, rapid cessation of medication, hypothermia
NCLEX Points
-
- Assessment
- Think HYPOmetabolic state
- Cardiovascular– bradycardia, anemia, hypotension
- Gastrointestinal– constipation (GI motility slows)
- Neurological– lethargy, fatigue (due to decreased metabolic rate—“body is slow and sleepy”), weakness, muscle aches, paresthesias
- Assessment
Integumentary- goiter, dry skin, dry hair, loss of body hair
-
-
- Metabolic– cold intolerance, anorexia, weight gain (due to decreased metabolic state), edema, hypoglycemia
-
Therapeutic Management
-
-
- Cardiac monitoring
- Maintain open airway
- Monitor medication therapy (overdose with thyroid medications possible)
- Medication therapy- levothyroxine (Synthroid)
-
Take in morning before breakfast to prevent insomnia (on empty stomach)
-
-
- Assess thyroid hormone levels
- IV fluids
- Monitor and administer glucose as needed
-
*Myxedema is COLD (hypothermia)
Hyperthyroidism- excess secretion of thyroid hormone (TH) from thyroid gland resulting in increased metabolic rate (accelerated physical and mental function)
- Causes
- Graves disease (autoimmune reaction)
- Excess secretion of TSH, tumor, medication reaction
Thyroid Storm (Thyroid Crisis)
-
- Extreme hyperthyroidism (life threatening) due to infection, stress, trauma
- Febrile state, tachycardia, HTN, tremors, seizures
- Extreme hyperthyroidism (life threatening) due to infection, stress, trauma
NCLEX Points
-
- Assessment
- Elevated T3, T4, free T4, decreased TSH, positive radioactive uptake scan
- Goiter
- Bulging eyes
- Cardiac- tachycardia, HTN (increased systolic, decreased diastolic), palpitations
- Neurological- hyperactive reflexes, emotional instability, agitation, hand tremor
- Sensory- exophthalmos (Graves disease), blurred vision, heat intolerance
- Integumentary- fine, thin hair
- Reproductive- amenorrhea, decreased libido
- Metabolic- increased metabolic rate, weight loss
- Assessment
Therapeutic Management
-
-
- Provide rest in a cool quiet environment
- Anti-thyroid medications (PTU, propylthiouracil)
- Cardiac monitoring
- Maintain patent airway
- Avoid drinks that are stimulants (increases metabolic rate)
- Caffeine- coffee, tea, soda
-
Provide eye protection
-
-
-
- Regular eye exams
- Moisturize eyes
- Radioactive Iodine 131
- Taken up by thyroid gland and destroys some thyroid cells over 6-8 weeks
- Avoid with pregnancy
- Monitor lab values for hypothyroidism
- Taken up by thyroid gland and destroys some thyroid cells over 6-8 weeks
- Surgical removal
-
-
Monitor airway
-
-
-
- Maintain in semi-Fowlers position
- Assess surgical site for bleeding
- Monitor for hypocalcemia
- Have calcium gluconate available
- Minimal talking during immediate post-op period
- (Partial-thyroidectomy) Monitor temperature post-op→ elevated temp by even 1 degree may indicate impending thyroid crisis→ report to MD immediately
-
-
*Think of MICHAEL JACKSON IN THRILLER
-Skinny, nervous, bulging eyes, up all night, heart beating fast
(Insomnia is aside effect of excess thyroid hormones—due to increased metabolic rate—body is “too busy to sleep”)
Hypo-parathyroid: decreased calcium (implement high calcium, low phosphorous diet; provide Vitamin D which aids in calcium absorption)
*Trousseau’s and Chvostek’s signs CATS (S/S):
C- convulsions A- arrhythmias T- tetany
S- spasms S- stridor
Hyper-parathyroid: increased calcium (implement low calcium, high phosphorous diet)
S/S: Fatigue, polyuria, muscle weakness, renal calculi (55% have urinary tract calculi), back and joint pain, monitor for bone deformities
Pre-parathyroidectomy- low calcium, high phosphorous diet
*For patients who are not candidates for para-thyroidectomy, diuretics (furosemide) and hydration (IV NS) in combo help reduce serum calcium → furosemide increases kidney excretion of calcium when combined with IV saline in large volumes
*BEST WAY TO EVALUATE FLUID STATUS (fluid volume deficit)- daily weight
Hypovolemia: (dehydration) increased temperature, rapid/weak pulse (tachycardia), increased respirations, hypotension, anxiety, urine SG > 1.030 (dark urine), confusion (early sign)
- Increased sodium with dehydration
- Increased BUN with dehydration
- Increased hematocrit with dehydration
Hypovolemic Shock
- Isotonic fluids – increase intravascular volume (NS or LR)
- Albumin can be given too (expander)
Hypervolemia: (fluid volume excess/overload) bounding pulse, SOB, dyspnea, crackles, peripheral edema, HTN, urine SG <1.010 (dilute urine); Semi-Fowler’s
*D5W-body rapidly metabolizes the dextrose and the solution becomes hypotonic
Low phosphorous—patient will exhibit generalized muscle weakness→ may lead to acute muscle breakdown (rhabdomyolysis)
- Phosphate is necessary for energy production in the form of ATP—when not produced, leads to generalized weakness
Diabetes Insipidus (DI): hyposecretion or failure to respond to ADH from posterior pituitary—leading to excess water loss
NCLEX Points
-
- Assessment (S/S)
- Excessive urine output
- Dilute urine (USG <1.006)
- Hypotension leading to cardiovascular collapse
- Tachycardia
- Polydipsia (extreme thirst)
- Excessive urine output
- Assessment (S/S)
Hypernatremia
-
-
- Neurological changes
-
Therapeutic Management
-
-
- Water replacement
-
D5W if IV replacement is required
-
-
- Hormone replacement
- Desmopressin
- Vasopressin
- Monitor urine output hourly and urine SG
- Report urine output > 200mL/hour
- Daily weight monitoring
- Hormone replacement
-
Syndrome of Inappropriate Antidiuretic Hormone (SIADH): excessive secretion of ADH (from posterior pituitary) leading to hyponatremia and water intoxication (excessive water retention)
- Caused by trauma, tumors, infection, medications
NCLEX Points
-
- Assessment (S/S)
- Fluid volume excess (HTN, crackles, JVD)
- Altered LOC
- Seizures
- Coma
- Urine specific gravity > 1.032
- Decreased BUN, hematocrit, Na (hyponatremia)
- Assessment (S/S)
Therapeutic Management
-
-
- Cardiac monitoring
- Frequent neuro exams
- Monitor I&O
- Fluid restriction
- Sodium supplement
- Daily weight (loss of 2.2 lbs or 1 kg = 1 L)
- Medication
- Hypertonic saline (D5 w/ NS)
- Diuretics (furosemide)
- Electrolyte replacement
-
*Water intoxication – drowsiness and altered mental status Specific Gravity
- 1.010-1.030
- High- (concentrated/dark urine)
- Dehydration
- SIADH
- Heart failure
- Low- (dilute/water-like urine)
- CKD
- Diabetes Insipidus
- Fluid volume overload
Hypomagnesemia (low Mg): tremors, tetany, seizures, dysrhythmias (life threatening ventricular arrhythmias), depression, confusion, dysphagia
*Low Mg may lead to digoxin toxicity
Hypermagnesemia (high Mg): depresses the CNS, hypotension, facial flushing, muscle weakness, absent deep tendon reflexes, shallow respirations
*Emergency
Addison’s Disease– hyposecretion of adrenal cortex hormones; decreased levels of glucocorticoids and mineralcorticoids leads to hyponatreamia, hyperkalemia, hypoglycemia, decreased vascular volume—fatal if not treated
NCLEX Points
-
- Assessment
- Hyponatremia (down)
- Hyperkalemia (up)
- Hypoglycemia (down)
- Decreased blood volume (down)- anemia
- Hypotension (down) – most important assessment parameter
- Weight loss
- Hyperpigmentation (tanned skin)
- Decreased resistance to stress
- Therapeutic Management – with Addison’s you must add
- Assessment
hormone (teaching about steroid replacement is important)
-
-
- Monitor vital signs
- Monitor electrolytes
- Monitor glucose
- Treat low blood sugar
- Administer replacement adrenal hormones as needed
- Lifelong medication therapy needed
- Managing stress in a patient with adrenal insufficiency is important—if the adrenal glands are stressed further it can result in Addisonian Crisis
-
Addisonian Crisis
-
-
- Caused by acute exacerbation of Addison’s Disease
- Causes severe electrolyte disturbances
- Monitor electrolytes and cardiovascular status closely
- Administer adrenal hormones as needed
- S/S: N/V, confusion, abdominal pain, extreme weakness, hypoglycemia, dehydration, decreased blood pressure
- During times of stress- increase sodium intake → a decrease in aldosterone leads to increase in excretion of sodium)
-
Cushing’s Disease– hypersecretion of glucocorticoids leading to elevated cortisol levels; greater incidence in women; life threatening if untreated
NCLEX Points
-
- Assessment
- Hypernatremia (up)
- Hypokalemia (down)
- Hyperglycemia (up)
- Increased blood volume (up)
- Hypertension (up)
- Prone to infection
- Moon face
- Buffalo hump
- Muscle wasting
- Edema (signs of CHF)
- Risk to bruising
- Assessment
- Therapeutic Management – you have excess “cushion” of hormones
- Monitor electrolytes and cardiovascular status
- Prevent fluid overload – respirations are the first priority
- Cardiovascular feature- capillary fragility→ results in bruising and petechiae
- Provide skin care and meticulous wound care (paper thin skin that is easily injured)
- Provide for client safety
- Adrenalectomy (surgical removal of adrenal gland)
- Protect client from infection
- Often caused by tumor on adrenal or pituitary gland
- Monitor electrolytes and cardiovascular status
Pheochromocytoma- vascular tumor of adrenal medulla (adrenal glands) leading to a hypersecretion of epinephrine/norepinephrine
- S/S: persistent HTN, increased HR, hyperglycemia, diaphoresis, tremor, pounding headache
- Management: avoid stress and frequent bathing, and take rest breaks (limit activity), avoid stimulating foods, avoid foods high in tyramine
- Avoid palpating the abdomen as it can cause a sudden release of catelcholamines and severe HTN
- Tx: surgery to remove tumor
Priority situation
Neuroleptic Malignant Syndrome (NMS)
NMS is like S&M
-You get hot (increased temp/hyperpyrexia)
-Stiff (increased muscle tone)
-Sweaty (diaphoresis)
-BP, pulse, and respirations go up
-You start to drool
*Flu like symptoms
*Never get pregnant with a German (German measles/rubella is the dangerous one for pregnant women)
- Exposure to rubella for a pregnant woman—incubation is 14 to 21 days (communicable 7 days before)
Pulmonary Embolism
- First sign- sudden chest pain, followed by dyspnea and tachypnea
- O2 deprived—first intervention is usually oxygen (check ABGs)
o Patient may be hyperventilating as a compensatory mechanism Risk Factors
- Obesity
- Immobility
- Pooling of blood in extremities
- Trauma (MVA)
Tetralogy of Fallot
*Think DROP (child drops to floor or squats) D- defect, septal
R- right ventricular hypertrophy O- overriding aorta
P- pulmonary stenosis
For neonates with Tetralogy of Fallot- prostaglandin E1 infusion
*Give O2 and morphine, IVF for volume expansion
MAOIs
*Pirates say “arrrr”—when pirates are depressed they take MAOIs
-MAOIs used for depression have an “ar” sound in the middle (parnate, marplan, nardil)
..or.. PANAMA
PArnate- tranylcypromine NArdil- phenelzine MArplan- isocarboxazid
*Avoid tyramine when taking MAOIs—aged cheese, chicken liver, avocados, bananas, meat tenderizer, salami, bologna, wine, beer—may cause HTN crisis
Systemic Lupus Erythematous- progressive systemic inflammatory disease resulting in major organ system failure; immune system “hyperactive” attacks healthy tissue; no known cure
NCLEX Points
-
- Assessment
- Assess for precipitating factors
- UV light
- Infection
- Stress
- Arthritis
- Weakness
- Photosensitivity
- Butterfly rash
- Elevated ESR and C Reactive Protein
- Assess for precipitating factors
- Assessment
Therapeutic Management
-
-
- Assess respiratory status
- Assess end organ function
- Plan rest periods
- Identify triggers
- Refer to dietitian for dietary assistance
- Medications
- Glucocorticoids
- NSAIDs
- Cyclophosamide (immunosuppressive agent)
-
**Should be in remission (SLE) at least 5 months prior to conceiving
*A high number of patients with SLE develop nephropathy, so an increase in blood urea may indicate a need for a change in therapy or for further diagnostic testing (such as creatinine clearance)
Albumin levels are the best indicator of long-term nutritional status (normal 3.5-5.0)
- (Same range as potassium)
One of the goals for a client with anorexia is to achieve a sense of self-worth and self-acceptance that is not based on appearance → encourage activities that will promote socialization and increase self-esteem
Physical S/S of anorexia
- Amenorrhea
- Constipation
- Hypotension
- Cold intolerance
- Bradycardia
- Fatigue
- Muscle weakness
- Osteoporosis
Autonomic Dysreflexia- potentially life threatening emergency (seen with patients with spinal cord injuries)
Elevate HOB to 90 degrees – FIRST
- Usually T6 or above spinal cord injury
- Vasoconstriction below
- Vasodilation above
- Sudden, acute onset of HTN
- Loosen constrictive clothing
- Assess for bladder distention and bowel impaction (can trigger AD)-
SECOND
- Administer anti-HTN medications (may cause stroke, MI, seizure
- Metallic bitter taste
Thrombolytic therapy- avoid injury→ avoid activities that could cause bleeding (NO IM injections)
*The Institute for Safe Medication Practices guidelines indicate that the use of a trailing zero is not appropriate when writing medication orders—because it is easily mistaken for a larger dose!
First action after medication administration error is to assess the client for adverse outcomes
Drug Schedules
- Schedule I- no currently accepted medical use, research only (heroin, LSD, MDMA)
- Schedule II- drugs with high potential for abuse and requires written prescription (Ritalin, hydromorphone/Dilaudid, meperidine/Demerol, and fentanyl)
- Schedule III- requires new prescription after 6 months or five refills (codeine, testosterone, ketamine)
- Schedule IV- requires new prescription after 6 months (benzodiazepines)
- Schedule V- dispensed as any other prescription or without prescription (cough preparations, laxatives)
Medication Considerations
Digoxin– assess pulse for a full minute, hold if HR less than 60, check digoxin levels and potassium and magnesium levels (low K and Mg can lead to digoxin toxicity)
S/S of toxicity- yellow halo, N/V
*Digoxin is given with loading doses (normally 2- 0.5mg or higher)—maintenance dose is typically 0.25mg
**Increases ventricular irritability—can convert a rhythm to V-Fib following cardioversion
Aluminum Hydroxide (Amphojel)– (antacid) treatment of GERD and kidney stones- watch for constipation
*Take after meals
Amiodarone- treats life-threatening heart rhythm problems; watch out for diaphoresis, dyspnea, lethargy—take missed dose any time in the day or skip it entirely—DO NOT take double dose
Warfarin (Coumadin)- anticoagulant therapy; watch for signs of bleeding, diarrhea, fever or rash; stress the importance of complying with prescribed dosage and follow-up appointments
- Patients taking warfarin should not make sudden dietary changes, because changing the oral intake of foods high in Vitamin K (green leafy vegetables, some fruits) will impact the effectiveness of the medication
Methylphenidate (Ritalin)- treatment of ADHD; assess for heart related side-effects and report immediately; child may need drug holiday because the drug stunts growth; poor appetite- parents should watch for weight loss
Ethambutol (TB)- negative effect on eyes (blurred vision, eye pain, red-green color blindness, any loss of vision—more common with high doses); liver problems may occur
Gemfibrozil– lowers high cholesterol and triglycerides; monitor liver functions
– increased risk of gallstones – rhabdomyolysis
Dextroamphetamine (Dexedrine)- used for ADHD, may alter insulin needs, avoid taking with MAOI’s, take in morning after breakfast (insomnia is a possible side effect)
Hydroxyurea– used to help treat sickle cell, can help reduce the number of acute chest syndrome episodes, pain crises, and need for blood transfusions—report GI symptoms immediately—could be sign of toxicity
Hydroxyzine (Vistaril)- tx of anxiety (can also be used to help with itching)- watch for dry mouth- commonly given pre-operatively
Haloperidol (Haldol)—preferred antipsychotic for elderly patients—high risk of EPS (dystonia, tardive dyskinesia, tightening of jaw, stiff neck, swollen tongue, swollen airway)—monitor early for signs of reaction (IM Diphenhydramine can be given)
- Side Effects- galactorrhea (excessive or spontaneous flow of milk), lactation, gynecomastia, drowsiness, insomnia, weakness, headache
- When given IM- should be given deep into large muscle mass—is very irritating to subcutaneous tissue
*If mixing antipsychotic medications (Haloperidol, Fluphenazine, Chlorpromazine) with fluids, incompatible with caffeine and apple juice
Risperidone (Risperdal)- antipsychotic (schizophrenia)—doses over 6mg can cause tardive dyskinesia—first line antipsychotic in children
- Causes weight gain, impairs temperature regulation, photosensitivity, orthostatic hypotension
Fluoxetine (Prozac)- SSRI; doses that are greater than 20mg should be given in divided doses
Midazolam (Versed)- given for conscious sedation- watch for respiratory depression and hypotension (benzodiazepine)
- Contraindicated in patients taking protease inhibitors
Protease Inhibitors– antiviral drugs used to treat HIV/AIDs and hepatitis C
*Decrease the metabolism of many drugs—including midazolam Serious toxicity can occur when protease inhibitors are given with other medications
Rifampin- (treatment of TB)- watch for red/orange tears, urine
*Decreases effectiveness of contraceptives
Propylthiouracil (PTU) and methimazole (tapazole)- prevention of thyroid storm
*Tx: hyperthyroidisim
Oxybutynin is an anticholinergic agent—can lead to extremely dry mouth; max dose is 20 mg/day; should be taken between meals as food interferes with absorption
Neostigmine- treats Myasthenia Gravis—administer to clients 45 min before eating—helps with swallowing and chewing
*Also reverses the effects of anesthesia
Procainamide HCl- given to treat PVCs- withhold if severe hypotension—adverse signs are bradycardia and hypotension
Isoniazid (medication for TB) causes peripheral neuropathy –patients may be instructed to take Vitamin B6 to counter; hepatotoxicity (monitor LFTs); should not be taken with Phenytoin (Dilantin) as it can lead to toxicity; hypotension may occur initially but should resolve
Trimethobenzamide HCl (Tigan)- tx of post-op N/V and for nausea associated with gastroenteritis
Alendronate– used for treatment and prevention of osteoporosis
- Photosensitivity- wear sunscreen and protective clothing when outdoors
- Take in the morning
- If missed dose, wait until next day to take
Doxycyline- antibiotic; dairy products inhibit the absorption of this medication
Cholestyramine- lower cholesterol
- S/E: constipation
- Should not take with spironolactone- increases blood chloride levels
- Many interactions- anticoagulants, beta blockers, diuretics, penicillins, hormonal contraceptives, phenobarbital
CBT– Can Block Tremors (meds for Parkinson’s)
Carbidopa/Levodopa (Sinemet)- sweat, saliva, urine may turn reddish brown, causes drowsiness; patients should not take with MAOIs
- Levodopa- contraindicated for patients with glaucoma, avoid Vitamin B6, avoid high protein diet (interferes with the body’s response to medication)
Benztropine (Cogentin)- can be used for Parkinson’s, as well as to treat EPS – may lead to the inability to move specific muscle groups or weakness (too much of an effect)—anticholinergic (may lead to blurred vision, dry mouth)
*Increase fluid intake
Biperiden– Anti-Parkinson’s used to counteract EPS
Trihexyphenidyl HCl (Artane)- sedative effect
Timolol (Beta Blocker)- eye drops, used for treatment of glaucoma
Propranolol (Beta Blocker)- decreases effectiveness of atorvastatin
Sulfamethaxozole/Trimethoprim (Bactrim)- antibiotic- do not take if allergic to sulfa- diarrhea is a common side effect, drink plenty of fluids
Simvastatin– tx of hyperlipidemia, take on empty stomach to enhance absorption at night, report any unexplained muscle pain (could indicate rhabdomyolysis)—especially if fever is present
Bromocriptine– used to treat menstrual problems
*Take with meals to avoid GI upset
Dabigatran- anticoagulant with NO antidote- do not take with other anticoagulants
Gout
Probenecid (Benemid)- increases uric acid secretion in urine
Colchicine– prevention of gout
Allopurinol– acute
Hydralazine– Tx of HTN or CHF, report flu-like symptoms, rise slowly from sitting/lying positions to prevent orthostatic hypotension, take with meals
Dicycloverine– Tx of irritable bowel- assess for anticholinergic side effects
Verapamil– CCB- tx of HTN, angina, and dysrhythmias- assess for constipation
Sucralfate– tx of duodenal ulcers (coats ulcer)- take before meals (1 hour)– best on empty stomach
*Protects from acid
Cimetidine– H2
*Take with meals and at bedtime S/E: constipation
Theophylline– tx of asthma and COPD
*Therapeutic drug level: 10-20 (12 letters in theophylline—12 is in between 10 and 20, also the “1” in 10 and “2” in 20 = 12)
N-Acetylcysteine– antidote for Tylenol and is administered orally
Glipizide– effective for client diagnosed with Type 2 DM, who produces minimal amounts of insulin (oral hypoglycemic agent)
Acetazolamide (Diamox)- tx of glaucoma, high altitude sickness, increased ICP- DO NOT take if allergic to sulfa
*Can cause hypokalemia
Indomethacin (Indocin)- NSAID- tx of arthritis (osteo, rheumatoid, gout), bursitis, tendonitis
*Ototoxic
Levothyroxine (synthroid)- tx of hypothyroidism- may take several weeks to take effect, notify doctor if chest pain—take in AM on empty stomach, can lead to hyperthyroidism
Chlordiazepoxide (Librium)- tx of alcohol withdrawal- do not take alcohol with this (including mouth wash that contains alcohol), very bad nausea and vomiting can occur
Terbutaline—can lead to maternal tachycardia- withhold if HR is elevated prior to administration
Vincristine (oncovin)- tx of leukemia (anti-leukemic)- IV only
Ganciclovir (Cytovene)- used for retinitis caused by cytomegalovirus- patient will need regular eye exams, report dizziness, confusion, or seizures immediately
Sertraline (Zoloft)- SSRI, depression; S/E: agitation, disruption in sleep, dry mouth
Serotonin Syndrome
-
- Rare, life threatening
- S/S: abdominal pain, fever, sweating, tachycardia, HTN, delirium, myoclonus (jerky movements), irritability, mood changes
Clozapine– schizophrenia; S/E: agranulocytosis (low WBC count), tachycardia, seizures
*Significant toxic risk associated with clozapine is blood dyscrasia Agranulocytosis- flu-like symptoms (fever, sore throat, lethargy)
Lindane (Kwell)- Tx of scabies (lotion) and lice (shampoo) Scabies- apply lotion once and leave on for 8-12 hours
Lice- wash hair with shampoo and leave on for 4 minutes with hair uncovered, then rinse with warm water and comb with a fine tooth comb
Dantrolene (Dantrium)- treats muscle spasms caused by MS—may take a week or more to be effective
Pentamidine– helps treat and prevent pneumocystis pneumonia
- Can cause fatal hypoglycemia—monitor blood glucose (low BG may indicate need to change treatment)
Doxepin HCl– antidepressant
*Signs of overdose: excitability and tremors
Premarin (conjugated estrogen tablets)- tx after menopause- estrogen replacement
*Estrogen can cause dry eyes
Furosemide (Lasix)- loop diuretic
- Ototoxic especially when given with other ototoxic drugs
- Monitor BP
- Monitor U/O
- Monitor K+
- Can lead to anorexia due to reduced potassium
Phenytoin (Dilantin)- tx of seizures
*Therapeutic drug level = 10-20
S/E: rash (stop med), gingival hyperplasia (practice good dental hygiene) Toxicity- poor gait + coordination, slurred speech, nausea, lethargy, diplopia Can cause leukopenia (low WBC)- stop medication
Thiothixene (Navane)- tx of schizophrenia- assess for EPS
Naproxen (NSAID)- used to mild to moderate pain
- Can cause gastrointestinal bleeding- monitor stools for blood
- Fluorouracil (5-FU)- chemotherapy agent
Sulindac (NSAID)– S/E are typically GI distress (GI bleeding, ulcers, perforation of the stomach and/or intestines)
Theophylline- used for COPD and asthma (bronchodilator)
-
- Causes GI upset, take with food
- Avoid use of alcohol and caffeine while taking this medication
- Watch for toxicity (10 to 20 is therapeutic range)- >20 is considered toxic (persistent nausea and vomiting are signs)
- Many drug interactions
Dopamine– treatment of hypotension, shock, low cardiac output, poor perfusion to vital organs (ex: kidneys)- monitor EKG for arrhythmias, monitor BP
Phenobarbital CAN be taken during pregnancy- phenytoin is contraindicated
*All psych meds (except Lithium) have the same side effects- SNS (exception is hypotension)
SNS- increase BP, HR, and RR, dilated pupils (blurred vision), urinary retention, constipation (decreased GI motility), constricted blood vessels, and dry mouth
Only specific medications require double verification
Epidural
-
- When doing epidural anesthesia, hydration beforehand is a priority
- Hypotension, bradypnea and bradycardia are major risks and emergencies
- Patients will have a foley catheter due to the inability to void
Forget your past mistakes and focus on your successes!
When caring for a pregnant woman who follows a vegetarian diet, the nurse should begin with an assessment of the diet (24 hour diet recall) because vegetarian practices vary widely—assess the diet for deficiencies before making recommendations for supplementation
Maternity Normal Values
-
- Fetal Heart Rate- 120 to 160 bpm
- Amniotic fluid- 500- 1200 mL
- APGAR- 7 and above = normal; 4 to 6 fairly low; 3 and below are critically low
- Done at 1 and 5 minutes
Prenatal vitamins should be taken with something acidic (orange juice) at bedtime (Vitamin C increases absorption)
Pregnant women should increase calories by 300 for fetal growth, maternal tissues and placenta
Placenta previa requires c-section
Hyperemesis gravidarum– bed rest, NPO to rest GI tract, anti-emetics, IVF
Symptoms of onset of labor
-
- Gush of fluid down legs
- Some blood in vaginal discharge
- Low back pain
Fetal Heart Rate Patterns
VEAL CHOP
VC EH AO LP
V= variable decels, Cord compression E = early decels, Head compression
A = accelerations, OK
L = late decels, Placental insufficiency (baby is not receiving enough oxygen and nutrients)
*For cord compression, place the mother in TRENDELENBURG position- this removes the pressure of the presenting part from the cord (baby is no longer being pulled out of the body by gravity)
-
- If the cord is prolapsed- cover it with sterile saline gauze to prevent drying of the cord and to minimize infection
*For late decels, turn the mother on the left side to allow more blood to flow to the placenta- give mother O2 via face mask, stop Pitocin, open IV fluids (increase)
*Sometimes it is hard to determine who to check on first, mom or baby—it is usually easy to tell the right answer if the mother or baby involves a machine—if you are not sure who to check on first, and one of the choices is a machine, that’s the wrong answer- eliminate
If the baby is in a posterior position- the sounds are heard at the sides
If the baby is in an anterior position- the sounds are heard closer to midline, between the umbilicus and where and where you would listen to a posterior position
*If the baby is breech- sounds are high up in the fundus (usually above or around the umbilicus)
*If baby is vertex (head is down), they are a little above the symphysis pubis on the left or right side
NEVER APPLY FUNDAL PRESSURE IN THE CASE OF SHOULDER DYSTOCIA!
A newborn discharged before 72 hours of life should be seen by an RN or MD within 2 days of discharge
A newborn should feed between 8 and 12 times in 24 hours
ALWAYS protect the newborn’s eyes when undergoing phototherapy and monitor temperature carefully! Breastfeeding is encouraged to avoid dehydration and increase passage of meconium (which helps excrete bilirubin)
Normal Contraction Pattern
-
- Contractions every 2-5 minutes for 60 seconds (<90 seconds)
- Longer lasting and shorter intervals is NOT normal (could be a complication of Pitocin)
- Contractions every 2-5 minutes for 60 seconds (<90 seconds)
Palpating uterine contractions is done with fingertips
AVA: The umbilical cord has two arteries and one vein
Amniotic fluid is alkaline- turns nitrazine paper blue
Urine and normal vaginal discharge are acidic and turn the nitrazine paper yellow/orange (some color charts vary)
If a woman’s water breaks and she is at a (-) station, you should be concerned about a potential prolapsed cord
Post-delivery
-
- Pitocin should only be administered after the placenta separates from the uterine wall
- Signs: gush of blood, umbilical cord out of vagina, uterus contracting
- Pitocin should only be administered after the placenta separates from the uterine wall
Umbilical cord care: clean cord several times a day and expose to air frequently (to encourage drying and prevent infection)
Oxytocin should always be a secondary infusion controlled by IV pump
Pregnancy weight gain:
-
- 2-5 lbs. in 1st trimester
- 0.6-1.1 lbs. weekly in 2nd and 3rd trimesters
Transition phase of labor- woman should pant with pursed lips→ allows client to control pain and urge to push and promotes adequate oxygenation of fetus

Other
- Methotrexate is teratogenic and should not be used by patients who are pregnant
Administration of antiviral medications to the pregnant woman and the newborn, cesarean birth, and avoidance of breastfeeding have reduced the incidence of perinatal transmission of HIV from approximately 26% to 1-2%
The incidence of congenital anomalies is 3x higher in the offspring of diabetic women—good glycemic control during preconception and early pregnancy significantly reduces this risk
A multiparous patient in active labor with an urge to have a bowel movement will probably give birth imminently—it is time to push—should not be allowed up to use the bathroom at this time!
Central Lines
- Jugular veins are more prone to infection
- Higher risk of infection with nontunneled lines
- PICC lines and midline catheters are associated with a lower incidence of infection
- Implanted ports are placed under the skin and are the least likely central line to be associated with catheter infection
VENTILATOR ALARMS HOLD
High pressure alarm- Obstruction due to increased secretions (mucus plug), kink in tubing, patient coughs, gags or bites
Low pressure alarm- Disconnection or leak in ventilator or patient airway cuff, patient stops spontaneously breathing
Increased ICP and Shock- OPPOSITE V/S
Increased ICP (Cushing’s Triad)- increased BP, decreased pulse (bradycardia), decreased respirations
Shock- decreased BP, increased pulse, increased respirations
Heroin withdrawal for a neonate
-Irritable
-Poor sucking
-High pitched cry
*Withdrawal seen 12-24 hours later
Heroin Withdrawal (Adult)
- Mimics S/S of fu- runny nose, yawning, fever, muscle and joint pain, diarrhea
JEWISH- No meat and milk together
Milk products and carbonated beverages have sodium For CPR of an infant – brachial pulse
Test child for lead poisoning around 12 months of age
Fruits high in potassium- bananas, potatoes, citrus fruits
*Cultures are always taken BEFORE starting IV antibiotics
A patient with leukemia may have epistaxis due to low platelets
Best way to warm a newborn: skin to skin contact on mother’s chest with a blanket
*Below 97.7 is a CONCERN
When patient comes to hospital in active labor- nurse’s first action is to listen to fetal heart rate
Phobic disorders-
Systematic desensitization- relaxation and gradual exposure to anxiety producing stimulus
GERD
- Risk Factors
- Female
- Smoking
- >45 years old
- Obesity
- Caucasian
- Limit spicy foods, caffeine, lie with 2 pillows
Low residue means low fiber
Fiber adds bulk- patients who are constipated should add fiber to their diet
High fiber– oatmeal, celery, green beans
Aminoglycosides (vancomycin and gentamicin) can cause nephrotoxicity and ototoxcity if given too quickly – monitor BUN and creatinine
“Red Man” syndrome occurs when vancomycin is infused too quickly—because the client needs the medication to treat infection, the vancomycin should not be discontinued—antihistamines my help decrease the flushing, but vancomycin should be administered over atleast 60 min!
ARDS (fluid in alveoli), DIC (disseminated intravascular coagulation) are always secondary to something else (another disease process)
- Cardinal sign of ARDS is hypoxemia (low oxygen level in tissues)
- First sign is usually increased respirations → later comes dyspnea, retractions, air hunger, cyanosis
Edema is in the interstitial space NOT in the cardiovascular space Weight is the best indicator of hydration status (dehydration) Wherever there is sugar (glucose), water follows
NO ASPIRIN TO CHILDREN– can cause Reye’s Syndrome (encephalopathy)
- S/S of Reye’s: vomiting, lethargy, unusual sleepiness, increased RR, diarrhea, confusion, loss of consciousness
ASPIRIN OVERDOSE SIGNS
- Tinnitus
- Gastric distress
COLD for acute pain (sprain, fracture), HOT for chronic pain (rheumatoid arthritis)
Pain is usually the highest priority for rheumatoid arthritis
Cultures taken before first dose of antibiotics Stool (+) – Salmonella → contact precautions
Detached retina- photophobia, loss of a portion of visual field
COPD is chronic, pneumonia is acute—emphysema and bronchitis are both COPD
- In COPD patients, baroreceptors that detect the CO2 level are destroyed—therefore, O2 level must be low because high O2 concentration blows the patient’s stimulus for breathing
- Ex: Patient is on O2 at 6L/min- this is too high→ causing high serum oxygen levels, which results in decreased respiratory rate
- Encourage pursed-lip breathing (promotes CO2 elimination)
- Encourage fluids
- High Fowler’s and leaning forward (tripod position)
Exacerbation- acute, distress
Gout- (acute attack)—encourage partial weight bearing
Epinephrine is always given in TB syringe
Prednisone toxicity→ Cushing’s syndrome – buffalo hump, moon face, hyperglycemia, HTN (too much steroid)
Prednisone Adverse Effects
- Osteoporosis
- Hyperglycemia (patient may require more insulin)
- Hypokalemia
- Hypernatremia
- Fluid retention and edema
- Decreased immune response (greater risk of infection—BUT do not see changes in bone marrow)
- Gastrointestinal bleeding—monitor stool for bleeding
*Rapid weight gain and edema are signs of excessive drug therapy and the dosage of the drug needs to be adjusted (contact physician to report)
Four options for cancer management: chemo, radiation, surgery, palliative/hospice (treatment/management can be a combination of these four)
Chest tubes are placed in the pleural space
- Placed to remove air/fluid from pleural cavity
- Creates a vacuum- NEGATIVE PRESSURE
- Air in the pleural space – pneumothorax
- Blood in the pleural space – hemothorax
- Should be below chest level
- Cough and deep breathing is encouraged
- 3 chambers
- Collection chamber
- Collects drainage- should be serosanguinous
- Assess drainage q4h (if new chest tube, assess more frequently)
- Notify MD if drainage is bright red (could indicate possible hemorrhage)
- Should not be more than 100mL/hour
- Collects drainage- should be serosanguinous
- Water seal chamber
- 2 cm of water
- Creates a one way valve that allows air to come out but nothing to go in
- Continuous bubbling is a bad sign→ air leak
- Should see gentle tidals (fluctuates with respirations)
- Suction control chamber
- Tells you how much suction is applied to the client
- MD sets the suction parameters
- Should see bubbling in suction chamber—means it is functioning properly
- Collection chamber
What NOT to do with Chest Tubes:
- Milk the catheter
 Never try to reinsert the tube if it is pulled out
Never try to reinsert the tube if it is pulled out
The immediate intervention after a sucking stab wound (open) is to dress the wound and tape it on 3 sides—allows air to escape but not reenter→ occlusive dressing would convert the wound from open to closed→ could lead to tension pneumothorax…which is worse!
*After dressing the wound: chest tube, labs, IV
Continuous bubbling indicates
air leak that must be identified:
- With the physician’s order, you can apply a padded clamp to the drainage tubing close to the occlusive dressing—if the bubbling stops, the air leak may be at the chest tube insertion, which will require you notifying the MD
- If the air leak does not stop when you apply the padded clamp, the air leak is between the clamp and the drainage system—you must now assess the system to carefully locate the leak
Angina (low oxygen to heart tissue) = no dead heart tissues
Myocardial Infarction (MI) = dead heart tissue present
- MI pain tends to be in morning hours
Blood tests for MI: myoglobin, CK and Troponin
- Troponin levels are elevated 3 hours after onset of MI- most specific to cardiac muscle injury or infarction
MONA- FIRST GIVE OXYGEN

*Most common complication following MI- arrhythmias (ventricular being the most serious)
Chest pain in a client undergoing a stress test indicates myocardial ischemia and is an indication to stop testing to avoid ongoing ischemia, injury, or infarction
Anti-cholesterol medications should be given with evening meal (at night)
Nitroglycerine is administered up to 3 times (every 5 minutes)—if chest pain does not stop- GO TO HOSPITAL or call 911—do not give if blood pressure is
<90/60
Preload affects amount of blood that goes to the right ventricle, afterload is the resistance the blood has to overcome to leave the heart
Calcium channel blockers affect afterload
- DO NOT DRINK GRAPEFRUIT JUICE WITH CCB
DO NOT GIVE BLOCKERS (BETA BLOCKERS, CALCIUM CHANNEL BLOCKERS) to PATIENTS WITH HEART BLOCKS
For a CABG, when the great saphenous vein is taken, it is turned inside out due to the valves that are inside
Unstable angina is not relieved by nitro
Prochlorperazine maleate (Compazine)- should be considered incompatible with all other medications in syringes
Angiotensin II is a potent vasodilator (from lungs)
Aldosterone attracts sodium
The past is gone- focus on the present and future!
REVERSAL AGENTS/ANTIDOTES
- Heparin = protamine sulfate
- Coumadin = vitamin K
- Ammonia = lactulose
- Acetaminophen = n-Acetylcysteine
- Magnesium sulfate= Calcium gluconate
- Iron = deferoxamine
- Digoxin = digibind
- TPA = aminocaproic acid (amicar)
- Methotrexate toxicity = leucovorin
- Alcohol withdrawal = Librium (Chlordiazepoxide)
- Opioids/Narcotics = Naloxone (Narcan)
- Methadone is an opioid analgesic used to detox patients addicted to narcotics
Low potassium potentiates digoxin toxicity (low Mg too) Heparin prevents platelet aggregation
COMMON NCLEX TOPIC
PT- 10- 14 seconds – therapeutic is 1.5 to 2 times
INR– 0.8 to 1.2- therapeutic is 2 to 3 times
PTT – 20-45 seconds- therapeutic is 1.5 to 2.5 times
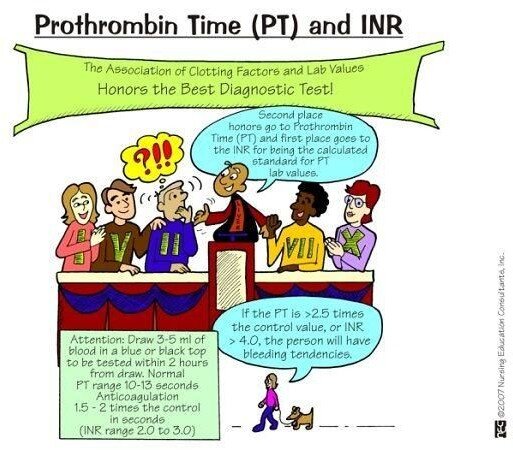
Oral anticoagulant therapy should be instituted 4-5 days before discontinuing heparin therapy
Cardiac output decreases with dysrhythmias- dopamine increases blood pressure
Med of choice for v-tach and PVCs is lidocaine
Med of choice for SVT and paroxysmal atrial tachycardia is adenosine
Med of choice for asystole is atropine
Med of choice for CHF is ACE-Inhibitor
Med of choice for burn pain management is morphine sulfate
Med of choice for candidiasis is ketoconazole
Med of choice for anaphylaxis is epinephrine
Med of choice for Status Epilepticus is benzodiazepine (valium, lorazepam) Med of choice for bipolar is lithium
- Increase fluid intake with lithium (2500-3000 mL/day)
- Maintain adequate salt intake (2-3 grams per day)
- S/E: increased U/O and dry mouth
- No ETOH with lithium
- Therapeutic level- 0.4 to 1.4
- Toxic level – 2 to 3: N/V/D, tremors (give mannitol and acetazolamide if signs of toxicity are present)
Amiodarone (anti-arrhythmic) is effective in both ventricular and atrial
complications
S3 (heart sound) is normal in CHF, not normal in MI
*May also hear S3 in fluid volume overload
Give sucralfate (anti-ulcer) before meals to coat stomach
Pantoprazole (Protonix) is given prophylactically to prevent stress ulcers (PPI)
Always check gag reflex following endoscopy
TPN is given via subclavian line (requires central line)
Diverticulitis (inflammation of the diverticulum in the colon)- pain in LLQ
- Can cause chronic or severe bleeding, if no obvious blood in the stool, the stool may be tested for occult blood
Bipolar Disorder
*Avoid competitive games when in manic phase (leads to increase in agitation)
Schizophrenia- inappropriate affect
ETOH Dependence
- Indication of need for more sedation- steadily increasing vital signs—client is approaching DTs
Appendicitis (inflammation of the appendix)- pain is in RLQ with rebound tenderness
Portal hypertension + albuinemia = ascites Beta cells of the pancreas produce insulin
Trousseau (carpal spasm with upper arm compression) and Chvostek’s sign
(facial nerve) are observed in hypocalcemia
- Chvostek- twitching- tapping face just below and in front of ear—neuro manifestation
Never give K+ in IV push Blood Transfusions
- ALWAYS ALWAYS ALWAYS NORMAL SALINE
- Use Y-connector
- Large-bore needle should be used (usually 20 gauge)
- Should be infused as soon as possible after they are obtained
- If patient presents with S/S of reaction- STOP the INFUSION!
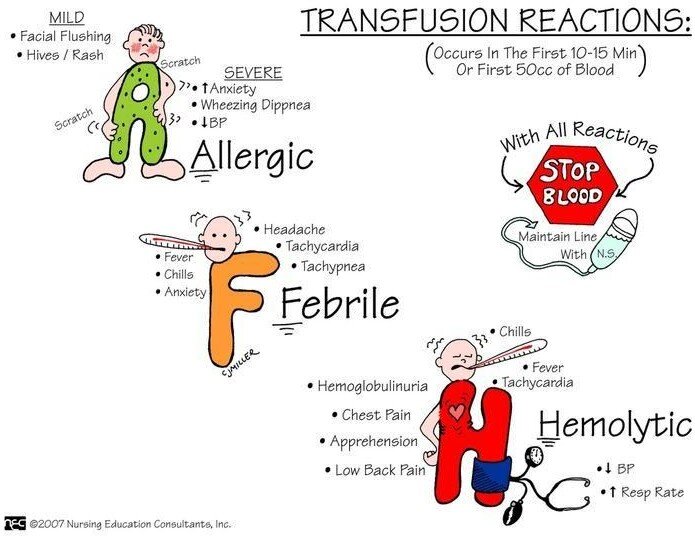
Types of Reactions
- Allergic- Mild facial flushing, hives/rash, increased anxiety, wheezing, dyspnea, hypotension
- Febrile- Fever, chills, anxiety, headache, tachycardia, tachypnea
- Hemolytic- N/V, pain in lower back, hypotension, tachycardia, decreased urinary output, hematuria, fever, chest pain
*FOR ALL REACTIONS- Stop infusion and maintain line with NS
Also supportive care (oxygen, Benadryl, airway), obtain urine specimen, blood product goes back to lab
Avoid douching before pap smear—affects appearance of cells in vaginal smear
Mineral (fludrocortisone- help manage bp) and glucocorticoids (hydrocortisone) are given in Addison’s disease
Sign of fat embolism– petechiae– treated with heparin For knee replacement- use CPM machine
Give prophylactic antibiotic therapy before invasive procedures
Glaucoma patients lose peripheral vision- treated with medications
Cataracts– cloudy, blurry vision – treated by lens removal-surgery

CO2 causes vasoconstriction
Most spinal cord injuries are at the cervical or lumbar regions
- Flaccid bladder- GOAL- want to promote acidic urine
- Client should drink cranberry juice, tomato juice, bouillon
Autonomic dysreflexia (life threatening- inhibited sympathetic response of nervous system to harmful stimulus- spinal cord injuries at T7 or above)- usually triggered by a full bladder
Spinal shock occurs immediately after spinal injury
Multiple Sclerosis– chronic progressive disease with destruction of myelin sheath, disruption in nerve impulse conduction—affects white matter of the brain and spinal cord
*Hyperactive deep tendon reflexes, vision changes, fatigue and spasticity are common symptoms – UTIs are common and may lead to sepsis
- Motor: limb weakness, paralysis, slow speech
- Sensory: numbness, tingling, tinnitus
- Cerebral: nystagmus, ataxia, dysphagia, dysarthria
Huntington’s Chorea- autosomal dominant disorder (50% chance of inheriting)
S/S: chorea (jerky, involuntary movement effecting shoulders, hips, and face); gait deteriorates with no ambulation, no cure, palliative
Guillan-Barre Syndrome = ascending paralysis (feet to head)- watch for respiratory system challenges
Parkinson’s = RAT → R- rigidity, A- akinesia (loss of muscle movement), T- tremors
- Tx: CBT (Can Block Tremors)- Carbidopa/Levidopa, Benzotropine, Trihexyphenidyl HCl
*Drooling in Parkinson’s is a concern—risk for aspiration (airway) Transient Ischemic Attack (TIA)- mini stroke with no dead brain tissue Cerebrovascular accident (CVA) – dead brain tissue
Hodgkin’s disease = cancer of lymph- very curable in early stages
Ranitidine – if taking once daily, should take at hour of sleep (absorption not affected by food)
When pulse rate drops in a patient with a pacemaker, it is cause for concern!
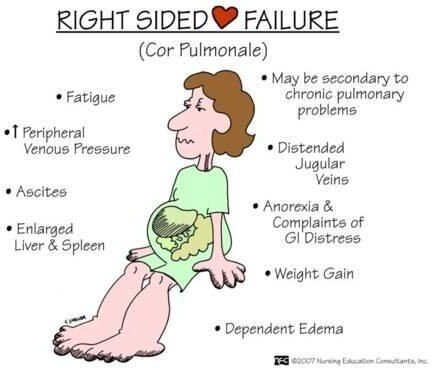
Polycythemia– increase in RBCs as compensation for decrease in oxygenation- seen in right-sided heart failure
Cor Pulmonae: right sided heart failure caused by left ventricular failure (S/S- edema, JVD)
Pulmonary sarcoidosis leads to right sided HF
DO NOT PICK COUGH over TACHYCARDIA for signs of CHF in an infant!
 Congestive Heart Failure
Congestive Heart Failure
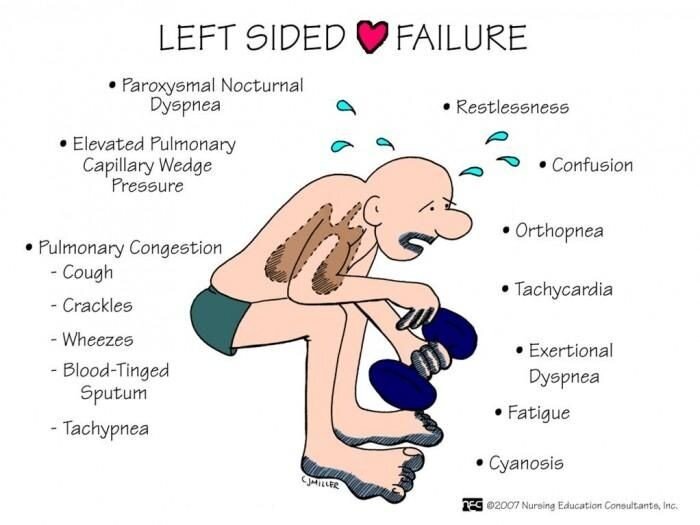
Ventricular gallop is the earliest sign of CHF
Early signs/stage of circulatory overload (seen in CHF) is change in character of respirations

Rule of Nines for Burns
m. 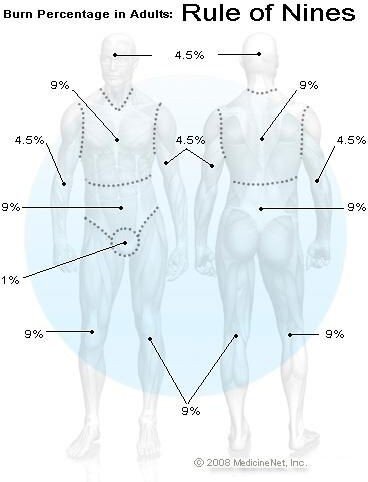
-
- Head & neck (front and back) = 9%
- Torso = 18% (upper/chest and lower/abdomen are each 9%)
- Back = 18% (upper back- 9%; lower back/buttocks – 9%)
- Each arm is 9%
- Each leg is 9%
- Groin/genitalia = 1%
*Example: If an adult had burns on both legs (9% + 9%), their groin (1%), and the chest (9%) and abdomen (9%) – 55% of their body is burned!
This rule helps guide treatment and fluid replacement! Parkland Formula– 4mL x kg body weight x % of total burned surface = amount of fluid to be infused over 24 hours
**Half that amount of fluid is to be infused over the first 8 hours (minus any fluid infused pre-hospital)
(Page 159 in ATI review book)
Priorities with Burns– 1) ABCs 2) Cardiac output 3) Fluids 4) Infection
Electrical burns– EKG
Chemical burn– do not touch until decontaminated (need to know the type of chemical)
Thermal burn– breathing is the #1 concern
Smoke– look inside nose for signs of smoke inhalation
*WITH BURNS TO FACE AND CHEST- BE CONCERNED ABOUT AIRWAY EDEMA
Important to maintain aseptic technique with burns- high risk of infection
Emergency care of partial thickness burns—remove clothing and wrap in clean sheet
*No soaps or ointments should be used in an emergency burn situation
BURNS
- 1st degree- red and painful
- 2nd degree- blisters
- 3rd degree- no pain because blocked and burned nerves

Birth weight doubles by 6 months and triples by 1 year of age
If HR is <100 in children, hold digoxin
Cystic Fibrosis- inherited by autosomal recessive trait
First sign of cystic fibrosis may be meconium ileus (bowel obstruction) at birth—baby is inconsolable, does not eat, does not pass meconium
- Respiratory problems are the chief concern
- Airway clearance techniques are critical (postural drainage/chest physiotherapy)
- Give aerosol bronchodilators, mucolytics and pancreatic enzymes
- Cystic Fibrosis- diet
- Low fat
- High sodium
- Fat soluble vitamins- ADEK
Heart defects– Cyanotic = 3 T’s (Tetrology of Fallot, Truncus arteriosus, transposition of the great vessels)—blood does not adequately return to the heart→ if problem does not fix itself, or cannot be corrected surgically, CHF will occur→ followed by death
With right-sided cardiac catheterization– look for valve problems
With left-sided cardiac catheterization– look for coronary complications
Rheumatic fever can lead to cardiac valve malfunctions/disease
*Group-A strep precedes rheumatic fever
- Patients experience chorea (grimacing, sudden jerky body movements)
- Joint pain is common
- Penicillin is usually given
- Watch for antistreptolysin O to be elevated
Cerebral palsy = poor muscle control due to birth injuries and/or decreased oxygen to brain tissues
Phenytoin (Dilantin) therapeutic level – 10-20; can cause gingival hyperplasia
Meningitis– nuchal rigidity, headache, photosensitivity, fever- Kernig’s and Brudzinski’s sign
*CSF in meningitis- high protein, low glucose
Wilm’s tumor– usually encapsulated above the kidneys- causing flank pain- DO NOT PALPATE THE ABDOMEN
Focus on your achievements rather than your failures—look at what you managed to do well and how you can improve!
Traction
Skin Traction
- Buck’s Traction- used to maintain proper alignment- hip fractures- want to maintain skin integrity and circulation
- Bryant’s
- Cervical halter
- Pelvic
Skeletal Traction
- Applied directly to a bone to reduce a fracture or maintain a surgically manipulated bone alignment
- Pins or wires inserted through skin and soft tissue into the bone
- Balanced suspension using splints, slings, weights
External Fixation Devices
- Rigid metal frames with attached percutaneous pins or wires used to align and immobilize
- Halo Traction- THINK SAFETY FIRST—always have a screwdriver nearby
*Place apparatus first, then place the weights when putting a patient in traction
Nursing Considerations for Traction
- Teach about movement
DO NOT ADJUST WEIGHTS (they should NEVER be on the floor—not exerting pulling force)
- Report pain (look for signs of compartment syndrome)
- Maintain skin integrity and circulation
*Nurse must always follow the chain of command – report to nursing supervisor or nurse manager
Compartment Syndrome- EMERGENCY SITUATION
- Paresthesia and increased pain are classic symptoms—neuromuscular damage is irreversible 4-6 hours after onset


A patient with a vertical c-section will more likely have another c/s
Perform amniocentesis (14-16 weeks) to check for fetal anomalies- Down Syndrome, Trisomy 18, Trisomy 13; detect presence of AChE in neural tube defects
*When it is performed late in pregnancy it can assess fetal lung maturity and fetal well-being
**Administer Rhogam to Rh- women
Rhogam is a blood product—as such, for NCLEX purposes, ONLY RN’s can administer Rhogam IM to client (do not delegate to LPN/LVN)

Indirect Coomb’s Test- Negative (normal) result means no antibodies are found; positive (abnormal) result means antibodies were found—DO NOT ADMINISTER RHOGAM TO A WOMAN WHO IS POSITIVE!
RhoGAM must be given prior to the Rh negative women
becoming sensitized… which is why RhoGAM is given prophylactically:
- During pregnancy (at 28-30 weeks) or any time the mother is exposed to fetal blood (such as after an amniocentesis, miscarriage, etc)
- Then after the birth of each Rh positive newborn, if no antibodies are identified in the mother (negative indirect Coombs), within 72 hours after delivery
Nagele’s Rule: Subtract 3 months and add 7 days to first day of last menstrual period
Anterior fontanel closes by 18 months
Posterior fontanel closes by 6-8 weeks
*Posterior closes before anterior
Caput succedaneum = diffuse edema of the fetal scalp that crosses the suture lines- swelling reabsorbs within 1-3 days
Pathological jaundice– occurs before 24 hours and lasts 7 days
Physiological jaundice- occurs after 24 hours
- Phototherapy considered for infant with total serum bilirubin >15 mg/dL at 72 hours of age
Placenta previa– bright red bleeding, no pain- NO VAGINAL EXAMS
Placental abruption– pain, no bleeding, rigid/board-like abdomen (monitor fluid volume stauts/I&O)
Betamethasone = surfactant- given to mothers in pre-term labor to help baby’s lungs mature before delivery – given in 2 doses (12-24 hours apart)
Magnesium sulfate– anticonvulsant for pregnant women with risk of seizures due to HTN
*Also used as a tocolytic to halt pre-term labor – contraindicated for women with myasthenia gravis, also with absent deep tendon reflexes
- Magnesium sulfate- (CNS depressant) can cause slowing of respirations and hyporeflexia; oliguria is another S/E
Oral (PO) medications are not recommended in labor—decreased GI motility
When breastfeeding- only wash breasts with water→ soap should be avoided as it causes dryness
Fundal height should correlate with weeks of pregnancy
*26 weeks = 26cm
Epigastric pain in pregnancy→ usually a sign of impending convulsion (according to Kaplan)
Crisis intervention = short term
FIVE INTERVENTIONS FOR PSYCH PATIENTS
- Safety
- Setting limits
- Establish trusting relationship
- Medications
- Least restrictive methods/environments to most restrictive
Most antidepressants take 3 weeks to take effect
Obsession = thought Compulsion = action
Hallucinations- redirect patient
Delusions- distract patient
Thorazine, Haldol (antipsychotics) can lead to EPS
Alzheimer’s disease is a chronic, progressive, degenerative cognitive disorder that accounts for more than 60% of all dementias
- Patient’s do not do well with short term memory
- Reality orientation- orient to what is going on right now
Safety and reorientation
- Place calendar and clock in obvious area
- Remind client of room and bathroom location
Atropine can be used to decrease secretions (drops)- blocks acetylcholine
- Holding pressure on the inner canthus (eye) decreases the amount of medication absorbed systemically (atropine drops)
*Atropine Overdose
- Hot as a Hare – elevated temperature
- Mad as a Hatter- change in LOC
- Red as a Beet- flushed face
- Dry as a Bone- thirsty
Decreased acetylcholine is related to senile dementia Dementia
- Geriatric client should be encouraged to talk about his life and important things in the past
Jill’s Favorite Medication:
Promethazine (Phenergan): anti-histamine; can be given as an antiemetic for nausea—crosses BBB—sedative effect – monitor fluid status (anticholinergic effects- anorexia, dry mouth and eyes, constipation, orthostatic hypotension)
Iron injections should be given Z-track method so they do not leak into SQ tissues Diazepam is commonly used as tranquilizer—to reduce anxiety before surgery Open wound in chest cavity– air needs to escape but not re-enter
*Three sided dressing
Auscultation of Heart Sounds- All– Aortic
Pigs– Pulmonic
Eat—Erb’s point
Too—Tricuspid Much—Mitral
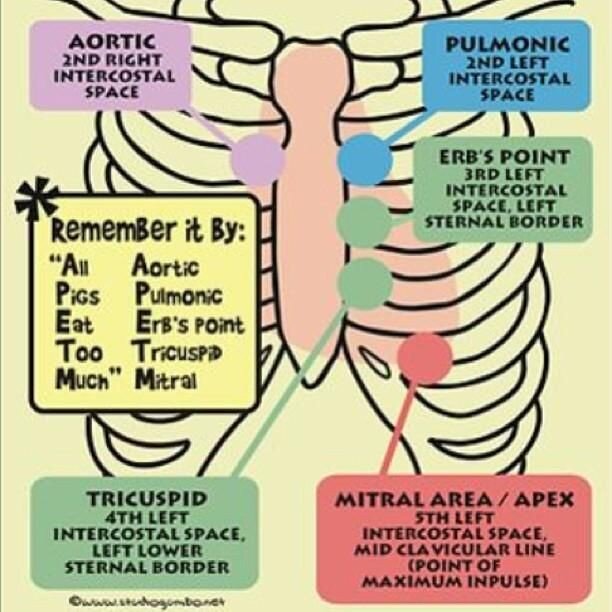
Cranial Nerves (mnemonic from “original GOLD”) Oh (Olfactory I) Some (Sensory)
Oh (Optic II) Say (Sensory) Oh (Oculomotor III) Marry (Motor) Tiny (Trochlear IV) Money (Motor) Tits (Trigeminal V) But (Both)
Are (Abducens VI) My (Motor)
Fun (Facial VII) Brother (Both) And (Auditory VIII) Says (Sensory) Give (Glossopharyngeal IX)Big (Both) Virgins (Vagus X) Bras (Both) Awkward (Accessory (XI) Matter (Motor) Hips (Hypoglassal XII) More (Motor)
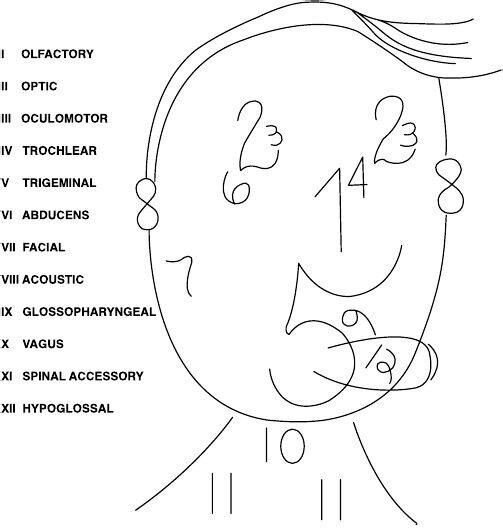

HYPERNATREMIA (greater than 145)
Skin flushed
Agitation
Low grade fever
Thirst
HYPONATREMIA (less than 135) Muscle twitching
Convulsions Diarrhea Headache Apprehension Lethargy
Developmental
2-3 months– demonstrates head lag, able to turn head up (can lift off mattress), tummy time, can turn side to side, cooing or gurgling noises and can turn head to sound, palmar grasp
4-5 months– rolls from back to side (4), places objects in mouth, rolls from front to back (5)
6-7 months– rolls from back to front, holds bottle/sippy cup, sits at 6 and waves bye/bye; can recognize familiar faces and knows if someone is a stranger, moves objects from hand to hand
8-9 months– stands straight at 8; sits unsupported, begins using pincer grasp, has favorite toy, plays peek-a-boo
10-11 months– crawling, changes from a prone to a sitting position (belly to butt), grasps rattles by its handles, finger foods
12-13 months– sits down from a standing position without assistance, starts walking (uses furniture to cruise), tries to build a two-block tower without success; cries when parents leave
*Twelve and up, drink from a cup
Hepatitis
-ends in a VOWEL and comes from the BOWEL (Hep A)
-Hepatitis B– Blood and Bodily fluids
-Hepatitis C is just like B
GLASGOW COMA SCALE
-Eyes, verbal, motor
*It is similar to measuring dating skills- max 15 points, one can do it! If below 8, you are in a coma
–To start dating, you have to open your EYES first- if you are able to do that spontaneously and use them correctly to SEE whom you are dating, you earn 4 points—but if she has to scream at you to make you open them it is only 3 points. If you dare not to open your eyes, even if she kicks you, you only get 1 point!
-If you get good EYE contact (4 points) then move on to VERBAL—talk to her/him, if you can do that you are oriented (4 points)—if you like her try not to be CONFUSED (3 points), and of course do not use INAPPROPRIATE WORDS (3 points) because she won’t like it—try not to respond with INCOMPREHENSIBLE SOUNDS (2 points)—but if you just don’t like her—do not respond at all- NO VERBAL RESPONSE (1 point)
-Since you now have EYE and VERBAL contact you can MOVE to Motor Response- this is VERY important, because good moves give you 6 points!
You’re simply the BEST- better than all the rest!
The person who hyperventilates is likely experiencing respiratory alkalosis
Avoid salt substitutes when taking digoxin and K-supplements—because they contain high levels of potassium
Signs of hypoxia: restless, anxious, cyanotic, tachycardia, increased respirations (also monitor ABGs)
For blood types: “O” is the universal donor (remember “O” in donor) “AB” is the universal recipient
**In emergency situations where typing and cross-matching have not yet been completed, “O“ can be given!
Medications to be given with food: NSAIDs, corticosteroids, medications for Bipolar Disorder, cephalosporins, and sulfonamides
When using a bronchodilator in conjunction with a glucocorticoid inhaler, administer the bronchodilator first!
Theophylline increases the risk of digoxin toxicity and decreases the effects of lithium and phenytoin
Peptic ulcers caused by H. pylori are treated with Metronidazole (Flagyl), Omeprazole (Prilosec), and Clarithromycin (Biaxin)—this treatment kills bacteria and stops production of stomach acid- it does not heal the ulcer!
A board-like abdomen with shoulder pain is a symptom of a perforation, which is the most lethal complication of peptic ulcer disease
Projectile vomiting can be a signal of obstruction in the GI tract
Diaphragm must stay in place for 6 hours after intercourse
*Also must be re-fitted if patient loses or gains a significant amount of weight!
Best time to take medications:
Growth Hormone (PM) Steroids (AM)
Diuretics (AM) – prevent nocturia
Donepezil (Aricept) (AM)- Alzheimer’s medication Cholesterol medications (PM)
Sulcrafate (before meals)- acts as a mucosal barrier—S/E: constipation Cimetidine (with meals and/or at bedtime)- many interactions
Antacids (1 hour after eating or when experiencing heartburn)- large amounts of antacid consumption can lead to osteoporosis
Glaucoma– intraocular pressure is greater than normal—give miotics to constrict (pilocarpine) – NO ATROPINE
- Tonometer is used to measure IOP and diagnose glaucoma
o Normal- 10 to 21 mmHg (according to Kaplan)
Dietary calcium- dairy products, seafood, nuts, broccoli, spinach
Non-dairy sources of calcium- RHUBARB, SARDINES, COLLARD GREENS
- Daily calcium intake- 1000 to 1500mg
With low back pain/aches, bend knees for pain relief (William’s position)
When taking allopurinol, patients should increase fluids to flush uric acid out of system!
Koplik’s spots are red spots (commonly found in mouth) with a bluish/whitish center—characteristic of PRODROMAL phase of MEASLES
Tuberculosis (TB)- medications must be taken for 6 to 9 months Endemic to Asia, Middle East, Africa, Latin America, Caribbean
A positive PPD confirms infection, not just exposure—a sputum test confirms active disease
PPD is (+) if induration is:
- >5mm for immunocompromised patients
- >10mm for high risk populations (IV drug users, recent immigrants, lab personnel, children <4 years)
- >15mm positive in any person (patients with no risk factors)
If a TB patient is unable/unwilling to adhere with treatment—may need supervision (direct observation) → TB is a public health risk
TB medications are toxic to the liver Adverse reaction is peripheral neuropathy
Most accidental eye injuries (90%) could be prevented by wearing eyewear for sports and hazardous work
Eye Drop Application
Apply eye drops to the conjunctiva sac—apply pressure to lacrimal duct/inner canthus (prevents systemic absorption)
Trendelenburg test for varicose veins—patient lies in supine position, leg is flexed at the hip and raised above the heart, the veins will empty due to gravity (or with the assistance of the examiner’s hand squeezing the blood towards the heart)—a tourniquet is then applied around the upper thigh to compress the superficial veins but not too tight as to occlude the deeper veins—the leg is then lowered and the patient is asked to stand. If the superficial veins fill more rapidly (than 30-35 seconds) with the tourniquet, there is valvular incompetence below the level of the tourniquet in the “deep” veins—after 20 seconds, if there is no rapid filling, the tourniquet is released—if there is sudden filling at this point, it indicates that the deep veins are competent but the superficial veins are incompetent!
*If superficial veins fill with tourniquet—deep veins are incompetent
*If there is sudden filling after tourniquet it removed—superficial veins are incompetent
Precautions when giving KAYEXALATE
- Assess for dehydration (K+ has inverse relationship with Na—when you decrease potassium, sodium increases)
- Assess patient for bowel sounds before administering—if hypoactive or absent bowl sounds—HOLD
- Monitor for electrolyte imbalances
- Interactions
- Caution with Digoxin (hypokalemia can lead to digoxin toxicity)
- Kayexalate may decrease the absorption of lithium
- Kayexalate may decrease the absorption of thyroxine
Yogurt has live cultures- do not give to immunocompromised patients
For itching under a cast- cool air via blow dryer, ice pack on cast for 10-15 minutes—NEVER stick anything in the cast to scratch the area
After PERITONEAL DIALYSIS– it is OKAY to have abdominal cramps, blood tinged outflow, and leaking around the site IF it was placed in the last 1-2 weeks—IT IS NEVER NORMAL to have CLOUDY OUTFLOW
Amniotic fluid- yellow with particles = meconium stained (baby is stressed)
Hyper-reflexes– upper motor neuron issue (“your reflexes are over the top”)
Hypo-reflexes (absent)- lower motor neuron issue
Order of Assessment– (IPPA) Inspection, Palpation, Percussion, and Auscultation→ EXCEPT with abdomen—you do not want to activate the bowels with your assessment so the order is: inspection, auscultation, percussion, palpation (also, if patient is presenting with abdominal problem, palpation and percussion may be painful so should be left for the end)
SIGNS
- Murphy’s Sign– pain with palpation of gall bladder area (seen with cholecystitis)
- Cullen’s Sign– ecchymosis in umbilical area, seen with pancreatitis (bruising)
- Turner’s Sign– ecchymosis (grayish blue) over flank areas- sign of pancreatitis (bad sign)
- McBurney’s Point– pain in RLQ indicative of appendicitis
- Rebound tenderness in RLQ—appendicitis
- RLQ pain– appendicitis, watch for peritonitis
- LLQ pain– diverticulitis (should maintain low reside diet, no seeds, nuts, peas)
- Guthrie Test– tests for phenylketonuria in newborns—babies should eat source of protein first
- Allen’s Test– occlude both ulnar and radial arteries until hand blanches, then release ulnar—if the hand returns to pink color—ulnar artery is good and you can use for ABG/radial arterial line/stick as planned—ABGs must be drawn in a heparinized tube, placed on ice and sent immediately to lab—should also inform lab of how much oxygen the patient is on (and via NC, mask, etc.)
- Schilling Test– tests for pernicious anemia—how well one absorbs Vitamin B12
 LATEX ALLERGY-
LATEX ALLERGY-
- Assess patient for allergies to bananas, apricots, cherries, grapes, kiwis, passion fruit, avocados, chestnut, tomatoes, peaches (also see above diagram)
Amyotrophic Lateral Sclerosis (ALS) is a condition in which there is degeneration of motor neurons in both the upper and lower motor neuron systems
Transesophageal Fistuala (TEF)– esophagus does not fully develop (this is a surgical emergency)
*The 3 C’s of TEF in newborn
- Choking
- Coughing
- Cyanosis
The MMR vaccine is given SQ not IM
-First dose recommended between 12 months and 15 months
-Contraindicated with allergy to gelatin and neomycin (also should not be given to immunocompromised patients because it is a live vaccine)
-Should not be given to pregnant women
-Because MMR is a live vaccine, it is not uncommon to spike a fever
Triage in Disaster/Mass-Casualty Situations
*Greatest good for the greatest number
Red- IMMEDIATE/EMERGENT: unstable, injuries are life threatening but survivable; do not delay treatment—airway, breathing, and circulation Ex: Airway obstruction, shock
Yellow- URGENT: major injuries that require treatment; can delay treatment 1-2 hours
Ex: Open fracture
Green- NONURGENT: minor injuries that do not require immediate treatment, can delay 2 to 4 hours
Ex: “Walking wounded”, closed fracture, contusions
Black– EXPECTANT: expected and allowed to die, prepare for morgue, comfort measures if possible
Ex: Profound hemorrhage, cardiac arrest
DOA– Dead on Arrival
Orange- psychiatric, non-urgent
Greek heritage- use of protective charms or amulet (necklace) around baby’s neck to protect against evil
4 year old kids cannot interpret TIME—they need time to be explained in relationship to a known common event—Ex: Mom will be back after supper
Allergies and Interactions
- Hep B Vaccine – should not receive if allergy to yeast
- Hep A Vaccine—should not receive if pregnant
- Flu shot—should not receive if allergy to eggs (also contraindicated for patient’s with a history of Guillain Barre)—OK to give to immunocompromised patients
- If a child has a cold, it is okay to give immunizations
- DTaP/Tdap– contradindicated with occurrence of seizures within 3 days of vaccine (possible adverse reaction- seizures)
- High fever 48 h after DTap is a valid contraindication for vaccine
- Rotavirus Vaccine- do not give if allergy to mycin drugs (aminogylcosides)
- Varicella Vaccine– should not receive if allergy to gelatin and neomycin or immunocompromised
- Meningococcal Vaccine– should not receive if history of Guillain Barre)
- HPV Vaccine– should not receive if allergy to yeast and/or pregnancy
- Penicillins and cephalosporins– crossover allergy (question orders of administering med if patient has documented/known allergy to either
- Aspirin and Naproxen– crossover allergies with NSAIDs
Adult Immunizations Schedule
- Tetanus booster- every 10 years
- MMR- one or two doses at ages 19 to 49
- Varicella- two doses if no history of disease
- Pneumococcal (PPSV)- once after the age of 65; recommended for immunocompromised, COPD, and living in long-term care facility
- Hepatitis A- two doses for high risk clients
- Hepatitis B and HPV- three doses for high risk clients (Hep B repeated @ 1 and 6 months)
- HPV should be given ideally before the patient is sexually active
- Seasonal influenza- annually; give to immunocompromised
- Meningococcal vaccine- students entering college, adults older than 65 repeat every 5 years for high-risk clients
- Herpes zoster- over age 60
Live Vaccines- do not give to immunocompromised and pregnant women
- MMR
- Varicella
- Nasal spray (flu)
When on nitroprusside, monitor thiocynate (cyanide)—normal value should be 1
→ >1 is heading towards toxicity
Severe Acute Respiratory Syndrome (SARS)—airborne and contact (just like varicella)
Hepatitis A is contact precautions
- Not infectious within a week or so after onset of jaundice Tetanus, Hepatitis B, HIV are STANDARD precautions Avoid high fat diet for Hepatitis B
NO VITAMIN C with ALLOPURINOL
No longer contagious after 24 hours of antibiotics
HIV
- Medications need to be taken very consistently—failure to take the medications daily can lead to mutations and the emergence of more virulent forms of the virus
- Viral load testing measures the amount of HIV genetic material in the blood, so a decrease in the viral load indicates that the HAART is effective
- Rapid HIV testing must be confirmed by another test, usually Western blot test
- Infants born to an HIV-positive mother should receive all immunizations on schedule
- A positive Western blot in a child < 18 months (presence of HIV antibodies) indicates only that the mother is infected – two or more positive P24 antigen tests will confirm HIV in children <18 months—P24 can be used at any age
- Kaposi’s sarcoma lesions should be cleaned and dressed daily to prevent secondary infection
- Avoid OPV (polio) and varicella vaccines in HIV + (both live)→ pneumococcal and influenza are OKAY
- MMR is only avoided if severely immunocompromised
- Parents should wear gloves for care, avoid sharing utensils and avoid kissing on the mouth (due to immunocompromised status—not for transmission purposes)
Signs of fractured hip: external rotation, shortening of affected leg, adduction
Rotavirus– spread via fecal-oral route- contact precautions for diapered and incontinent patient’s
Fat embolism– blood tinged sputum (related to inflammation), elevated ESR, respiratory alkalosis (related to tachypnea), hypocalcemia, increased serum lipids, “snow storm” effect on chest X-ray
Complications of Mechanical Ventilation– pneumothorax, ulcers, pneumonia (ventilator associated)
Paget’s Disease-abnormal bone destruction and regrowth; cause unknown (may be genetic or due to virus early in life)
*S/S: tinnitus, bone pain, enlargement of bone (though weak/soft), headache, hearing loss, reduced height, bowing of the legs, hypercalcemia
Intravenous Pyleogram (IVP)- requires bowel prep in order to better visualize the urinary tract (bladder, kidneys, ureters, urethra)
Acid Ash Diet- meat, poultry, cheese, fish, eggs, grains, cranberries, prunes, plums
Greenstick fractures are commonly seen in children (also known as buckle fractures)—bends on one side and cracks on the other
BOTOX can be used for strabismus (12 and older)—patch the GOOD eye to allow the weaker eye to get stronger
COPD patients- 2L via NC or less (hypoxic not hypercapnic drive), PaO2 in 60’s and SaO2 of 90% is normal—chronic CO2 retainers
Amphotericin B- (Amphoterrible): treats infection caused by a fungus
*Should only be given to patients with severe, life threatening fungal infection Side Effects: fever (common), hypokalemia
*Must premedicate- Tylenol and Benadryl can be used
Mebendazole (Vermox) is used to treat worm infections (pinworms, roundworms, hookworms)—increase fat in diet to increase absorption
Kidney glucose threshold is 180—when the blood glucose levels exceed
160-180 mg/dL, the proximal tubule becomes overwhelmed and begins to excrete glucose in the urine
Glucose Tolerance Test for pregnant women- results of 140 or higher needs further evaluation
Lymes is found mostly in Connecticut
For asthma and arthritis—swimming is best
Intercostal retractions and asthma—BE CONCERNED – also, if the asthma patient in the waiting room becomes silent—wheezer stops wheezing (RED FLAG)
Coughing without other S/S is suggestive of asthma
Increased pulse rate with asthma—indicating decreased oxygenation
Tardive Dyskinesia– irreversible, involuntary movements of the tongue, face, and extremities—may happen after prolonged use of antipsychotics
Akathisia– motor restlessness; treated with Anti-Parkinson medications—can sometimes be mistaken for agitation
Before Pulmonary Function Tests (PFTs)—bronchodilators should be withheld and they are not allowed to smoke for 4 days prior
For a lung biopsy—position patient on side of bed with arms raised up on pillows over bedside table—have patient hold breath in mid expiration, chest x-ray is done immediately to check for complications (pneumothorax)—sterile dressing is applied- patient should lie on right side following biopsy
EEG– before–hold medications 24-48 hours prior (anti-seizure medications), no caffeine or cigarettes for 24 hours prior, patient can eat, must stay awake the night before the exam—during exam patient may be asked to hyperventilate and watch a bright flashing light—after exam- assess patient for seizures, patient is at an increased risk
Decorticate– towards the cord
Decorticate positioning in response to pain = CORtex involvement
Decerebrate– away from body
Decerebrate positioning in response to pain = CEREBellar, brain stem involvement
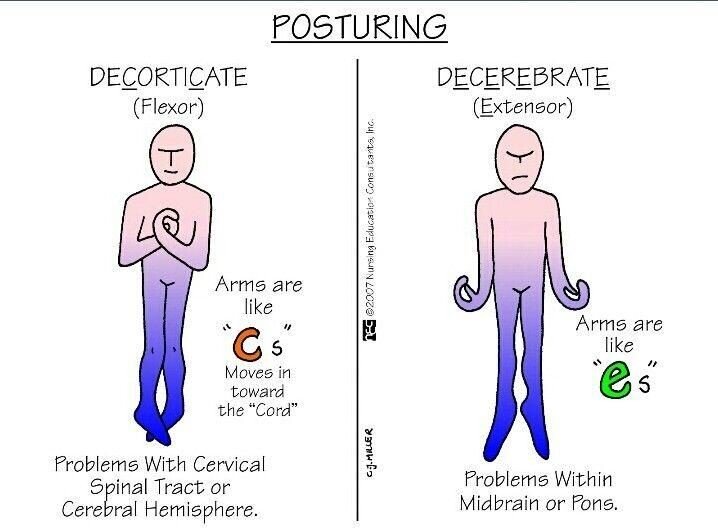
*Definitive diagnosis for Abdominal Aortic Aneurysm (AAA)- CT Scan
WBC– shift to the left means there are a high number of immature white blood cells present—most commonly this means there is an infection or inflammation present and the bone marrow is producing more WBCs and releasing them into the blood before they are fully mature
Chronic Kidney Disease (Renal Failure)
- Progressive, irreversible loss of renal function with associated decline in GFR
- All body systems affected- dialysis is required
- End stage renal disease occurs with GFR <15 mL/min
- Causes:
- DM (leading cause)
- HTN (second cause)
- Unreversed acute kidney injury
- Glomerulonephritis
- Autoimmune disorders
NCLEX Points
-
- Assessment
- Azotemia (elevated BUN and creatinine)
- Cardio– HTN, hypervolemia, CHF
- Hematologic– anemia, thrombocytopenia
- Gastrointestinal– anorexia, N/V
- Neurological– lethargy, confusion, coma
- Urinary– decreased urine output, proteinuria
- Skeletal– osteoporosis
- Assessment
Therapeutic Management
-
-
- Epoetin alfa aids in countering anemia
- Avoid administering aspirin
- Monitor K levels
- Elevated potassium can lead to EKG changes (peaked T waves, flat P, wide QRS, blocks, asystole)
- Provide low potassium diet
- Potassium lowering medications
- Kayexalate
- Insulin
- Calcium gluconate
- Continuous cardiac monitoring
- Phosphate binders may be required to lower phosphorous levels
- Monitor daily weights
- Monitor for signs of heart failure
- Monitor electrolyte levels (will see low magnesium) and BUN/Creatinine
- Assess peripheral nerve function and monitor for peripheral neuropathy
- Vision can be affected- monitor and provide for a safe environment
- Instruct client on dialysis and provide end of life care as needed
-
- Stage I- diminished kidney reserve → function is reduced but healthier kidney is able to compensate (polyuria and nocturia)
- GFR >90mL/min
- Stage II
- GFR 60 to 89 mL/min
- Stage III
- GFR 30 to 59 mL/min
- Stage IV
- 15 to 29 mL/min
- Stage V (End Stage Renal Disease)
- <15 mL/min
Hemodialysis– process of cleansing the blood of accumulated waste products and fluids—used for ESRD or for the acutely ill that require short-term treatment
- Hold meds prior to hemodialysis
- Monitor BP- concerned about BP
- Check circulation
- Weigh before and after
- AV Fistula
- Auscultate for whooshing sound over fistula (bruit and thrill), palpate for warmth and tenderness
- No weight on extremity
- No BP or blood work from fistula side
- Do not lift heavy objects
Peritoneal Dialysis– alternative method using the peritoneum to remove fluids, electrolyte, and waste products from the blood
- Warm dialysate
- Allow to flow in by gravity
- 5-10 min inflow time- close clamp immediately
- 30 min of equilibriation (dwell time)
- 10-30 min of drainage (should be clear and pale yellow)
- Monitor for complications: peritonitis, bleeding, respiratory difficulty, abdominal pain, bowel or bladder perforation
Continuous Ambulatory Peritoneal Dialysis (CAPD)
- Permanent indwelling catheter inserted into peritoneum
- Fluid infused by gravity (1.5 to 3L)
- Dwell time- 4 to 8 hours
- Dialysate drains by gravity- 20 to 40 min
- Four to five exchanges daily (7 days/week)—some elect to do it at night
- Full colon can create outflow problems
Uremic Fetor– urine smelling breath (seen in patients with uremia—elevated serum urea level)—seen in chronic kidney disease
Normal Creatinine– 0.6 to 1.2
Normal BUN– 10 to 20 (some sources say 9 to 20)
Normal GFR– 85 to 135 (<80 indicates decreased function)
Clients with kidney disease are susceptible to CNS effects (confusion and dizziness)—dosage my need to be reduced
Signs and Symptoms of Kidney Rejection
- Diffuse pain over kidney (tenderness)
Congenital Gastrointestinal Disorders Hypertrophic Pyloric Stenosis- projectile vomit
- Thickening of pyloric sphincter; genetic
- Manifestations: vomiting that occurs 30-60 min after a meal and becomes projectile as obstruction worsens
- Constant hunger
- Olive-shaped mass in RUQ
- Peristaltic wave that moves left to right when lying supine
- Failure to gain weight and signs of dehydration
Nursing Interventions
-
- Place child on side with head elevated when vomiting to prevent aspiration
- Daily weight and I&O
- Monitor fluid and electrolyte balance to assess for deficits
- IV fluid replacement as needed
o NPO
o Monitor NG tube
Therapeutic Management
-
- Surgical incision into the pyloric sphincter (pylorotomy)
Hirschsprung’s- failure to pass meconium, ribbon-like stool
- Occurs when a section of the colon is aganglionic – absence of ganglion cells (nerves that contribute to peristalsis)—problem that prevents stool from moving forward in the GI tract
Manifestations
-
- Newborn– failure to pass meconium within 24-48 hours, refusal to eat, episodes of bilious vomit, abdominal distention
- Infant- failure to thrive, constipation, abdominal distention, episodes of vomiting and diarrhea
- Older child- constipation, abdominal distention, ribbon-like stool, palpable fecal mass, malnourished
Nursing Interventions
-
- Position child on side or with head elevated when vomiting to prevent aspiration
- Monitor fluid and electrolyte balance to assess for deficits
- Provide oral care after vomiting
Therapeutic Management
-
- Surgical removal of the aganglionic section (colostomy may be temporary)
- Serial rectal irrigation may be used to decompress bowel prior to surgery
Intussusception- bloody stool (red currant jelly)
- Telescoping of the intestine upon itself; not a congenital condition but often occurs with congenital conditions such as cystic fibrosis
Manifestations
-
- Normal comfort interrupted by periods of sudden and acute pain
- Palpable, sausage-shaped mass in RUQ of abdomen and/or tender, distended abdomen
- Stools that are mixed with blood and mucus (red currant jelly)
Nursing Interventions
-
- Position child on side or with head elevated when vomiting to prevent aspiration
- Monitor fluid and electrolyte balance to assess for deficits
- Assess for currant jelly stools
Therapeutic Management
-
- Surgical reduction if inflating the bowel with air or administering barium enema is not successful
- Proton Pump Inhibitors (Omeprazole)
- H2 Receptor Antagonists (Ranitidine)
Cleft Lip (CL) and Cleft Palate (CP)- aspiration
- Multifactorial, but there are strong indicators of genetic or environmental factors
- Cleft palate is more common in males
- Cleft lip is more common in females (THINK: you are able to better visualize cleft lip externally—females generally care more about their appearance—therefore, cleft lip is more commonly seen in females)
Manifestations
-
- Cleft lip is visible
- Cleft palate alone may only be visible when examining the mouth
- Individuals are prone to ear, nose, and throat infection
- Long-term problems include speech, hearing, and dentition problems
Nursing Interventions
-
- Assess respiratory status and ease of respiratory effort
- Keep suction equipment and bulb syringe at bedside
- Assess ability to suck and swallow
- Modify feeding techniques utilizing obturators, special nipples, feeders
- Feed in upright position in frequent, small amounts, burp frequently
- Daily weight and monitor I&O
Therapeutic Management
-
- Repair usually completed by 12 to 18 months of age to prevent speech problems
- Surgery may be performed in stages
Avoid Vitamin C prior to occult stool test- can lead to false +
All activities that the client participated in before a colostomy may be resumed after appropriate healing of the stoma and incisions
Hypospadias- abnormality in which the urethral meatus is located on the ventral aspect of the penis (below)
Epispadias- abnormality in which the urethral meatus is located on the dorsal side of the penis (top)
Priapism– painful erection lasting longer than 6 hours
Mastectomy- complaints of “wet sheets” – could indicate hemorrhage from operative site
Thank You Mary- Anticholinergic Effects Can’t Spit- dry mouth Can’t Shit- constipation
Can’t Pee- urinary retention Can’t See- blurry vision
When you see coffee-brown emesis—think peptic ulcer Fluid retention- think heart problems first!
Erikson’s Stages of Psychosocial Development
- Infants- 0 to 1 year
- Trust vs. Mistrust- trust develops as needs are met
- Toddlers- 1 to 3 years
- Autonomy vs. Shame and Doubt- toddlers want to make choices
- Preschooler- 3 to 6 years
- Initiative vs. Guilt- guilt may occur if unable to successfully complete a task or if they are “punished” for an unsuccessful try
- School-Age Child- 6 to 12 years
- Industry vs. Inferiority- a sense of industry is achieved through advancements in learning; fears of ridicule are common
- Adolescent- 12 to 20 years
- Identity vs. Role Confusion- families strongly influence personal identity, peer groups greatly influence behavior, interest in opposite sex, career planning, may see themselves as invincible
- Young Adult- 20 to 35 years
- Intimacy vs. Isolation- ability to love deeply and commit oneself in relationships vs. remaining uncommitted and alone
- Middle Adult- 35 to 65 years
- Generativity vs. Stagnation- ability to give and care for others vs. self-absorption and inability to grow as a person
- Older Adult- 65 years and older
- Integrity vs. Despair- sense of accomplishment in life vs. feeling dissatisfied with life
Fetal Alcohol Syndrome
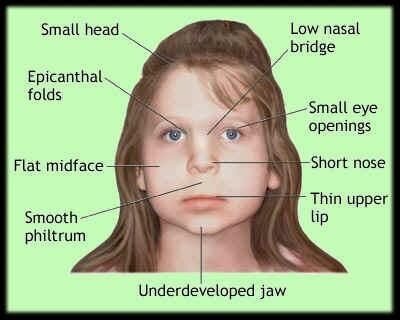
IM administration for 6 month old infants- vastus lateralis
IM administration for toddlers (>18 months)- ventrogluteal
IM administration for children- deltoid and gluteus maximus
Eye Abbreviations OU-both eyes
OS– left eye
OD– right eye (dominant side is usually right side- right eye)
Ear Abbreviations AU- both ears
AS- left ear
AD- right ear( dominant side is usually right side- right ear)
COAL
Cane Opposite Affected Leg
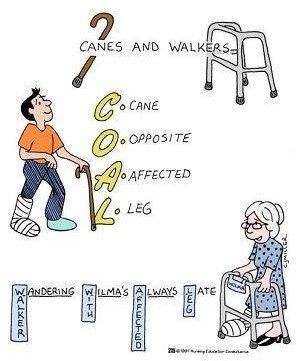
Walker
Wandering- Walker Wilma- With Always- Affected Late- Leg
Stand slightly behind the patient using a cane (on strong side)
For CT scan- assess for allergies to contrast (allergy to shellfish) MRI- claustrophobia, NO METAL
- Contraindicated for patients with pacemaker, stents, cochlear implants, surgical implants
- Titanium joint replacements CAN have MRI
- Remove transdermal patches prior to MRI
Cardiac Catheterization
- NPO 8-12 hours prior
- Empty bladder
- Check pulses and mark
- Tell patient he may feel palpitations or desire to cough with dye
- Post- V/S, keep leg straight (insertion site is typically in groin), maintain bed rest 6-8 hours
Early Signs of Increased ICP
- Pupil changes
- Change in LOC/mental status changes
Increased ICP in Infants/Neonates
- High pitched cry
Intracranial Pressure (ICP) should be < 20 mmHg –measure head circumference—Normal ICP is usually between 10-15 mmHg (opening pressure)
Early Signs of Subdural Hematoma and Cerebral Edema
- Decreased level of consciousness
- Ipsilateral pupils (same side as hematoma)
- Headache – usually the first symptom
NO MORPHINE WITH HEAD INJURY- MASKS SIGNS OF INCREASING ICP
Fixed and dilated pupils represents a neuro emergency
Clear fluid draining out of ear indicates rupture of meninges and presents a possible complication of meningitis
Self-catheterization (urine)- clean procedure (not sterile)
Strabismus– sign: child closes one eye to see a poster on the wall—visual axes are not parallel so the brain receives two images
Cholecystectomy
- Do not need to restrict fat post-op
T-Tube
- Post-cholecystectomy
- Used to drain bile—if change in urine color, bile is draining into the liver
- Should not be irrigated, aspirated or clamped without a specific order from the physician
Hemovac– closed system (requires negative pressure)
- Used often after mastectomy
- Empty when full or q8h
- Remove plug, empty contents, place on flat surface, cleanse opening and plug with alcohol sponge, compress evacuator completely to remove air, release plug, check system for operation
Anthrax-not spread person to person (can be spread from contaminated clothing—so patients should undergo decontamination—removal and disposal of clothing and showering is the initial action in possible anthrax exposure)
- According to the CDC, antibiotics should be administered only if there are signs of infection or the contaminating substance tests positive for anthrax (LaCharity)
- Ciprofloxacin is the antibiotic used to combat anthrax
- Teaching for Ciprofloxacin
- Drink plenty of fluids
- Avoid taking a multivitamin within 6 hours of taking this medication
- Avoid exposure to sun
- Avoid caffeine
- May take with meals
- Teaching for Ciprofloxacin
- Ciprofloxacin is the antibiotic used to combat anthrax
Generally speaking, exposure does not mean active disease
Lactose Intolerant-
- Foods high in calcium but no dairy/milk products
Tracheostomy
- Fenestrated (cuffed) tracheostomy
- When capping a fenestrated cuff—deflate the cuff first
- 80-120 mmHg wall suction pressure
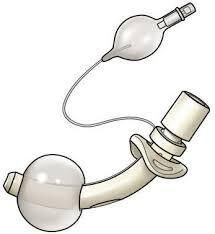

Vasectomy
- No permanent effect on sexual function
- Should use condom for first 6 weeks post-op V-fib, defibrillate
You are at risk for developing cervical cancer if you have/had multiple sex partners
Women who begin menstruating at an early age (such as 9 years old), are at risk for breast cancer
Absence of menstruation leads to osteoporosis in the patient with anorexia
24 hour urine specimen collection
- If a woman starts menstruating during the collection—contact physician
It is not unusual for an adolescent who just started menstruating to not have a period every month (usually expect to have around 4 in the first year)
Breast buds usually appear between 9-13 years of age—should be investigated if they appear later
Glucagon (1mg SQ) is given when patient is unconscious with severe
hypoglycemia or those who cannot take PO fluids
*Increases the effects of anticoagulants
Crohn’s Disease
- Low fat
- Low residue (fiber)
- High protein
Priority assessment- respiratory distress
- Listen to patient’s breath sounds (most clear assessment)
Femoral angiogram– locate and note the presence of peripheral pulses (easier to find after the procedure)
- Keep leg straight
- Check dressing
- Increase hydration to excrete dye
Breath Sounds
- Asthma
- High-pitched, musical sounds on expiration (wheezing)
- Pneumonia
- Soft, high-pitched sounds on inspiration (crackles)
- Bronchitis
- Deep, low-pitched rumbling on expiration (rhonchi)
Ileostomy- seen with spinal cord injuries, Crohn’s disease, and to rest the colon
- Clean with warm water, dry thoroughly
- Appliance should fit snugly around the opening
- Should not take laxatives
- Can take multi-vitamins
- No enteric coated meds or capsules—breakdown in large intestines
- Stoma site should be assessed at least once a day
- Bags can be changed as needed
- Liquid stool
*DO NOT CONFUSE ILEOSTOMY WITH COLOSTOMY*
Maintain bathroom schedule for incontinent patients- every 2 hours
When transferring a patient to another unit—you do not want to bring a “threat” to the floor—clean vs. dirty patient—risk of infection to a “clean” unit is not a good choice
For the initial dose of an ACE-Inhibitor—should not give with diuretics and other medications that can decrease blood pressure (with the initial dose, hypotension is concern)
Oral fluid intake—1500 mL in 24 hours
Patient who is agitated- reorient to place and time, assign LPN to stay with patient
In pH regulation, two organs of concern are lungs and kidneys (lungs- respiratory, kidneys- metabolic)
ARTERIAL BLOOD GASES
*Risk factors for acid-base imbalances include chronic kidney disease and pulmonary disease
Metabolic Acidosis
- Low pH, Low HCO3
Risk Factors
-
- Type 1 Diabetes (at risk for DKA)
- Salicylate toxicity
- Acute renal failure (decreased production of HCO3)
- Severe diarrhea
- Hyperkalemia
Metabolic Alkalosis
- High pH, High HCO3
Risk Factors
-
- GI losses- vomiting or gastric suctioning or drainage
- Nasogastric suctioning can result in a decrease in acid components leading to metabolic alkalosis—clients decrease in rate and depth of ventilation in an attempt to compensate by retaining carbon dioxide
- Diuretic therapy that leads to sodium and chlorine losses
- Mineralcorticoid excess
- Hypokalemia
- GI losses- vomiting or gastric suctioning or drainage
Respiratory Acidosis
- Low pH, High PaCO2
Risk Factors
-
- Respiratory depression (decreased respiratory rate)
- COPD and/or asthma
- Inability to ventilate properly (seen in myasthenia gravis, ALS, muscular dystrophy, and Guillain Barre)
Respiratory Alkalosis
- High pH, Low PaCO2
Risk Factors
-
- Hyperventilation (blowing of CO2)
- Mechanical ventilation
- Any condition that causes shortness of breath
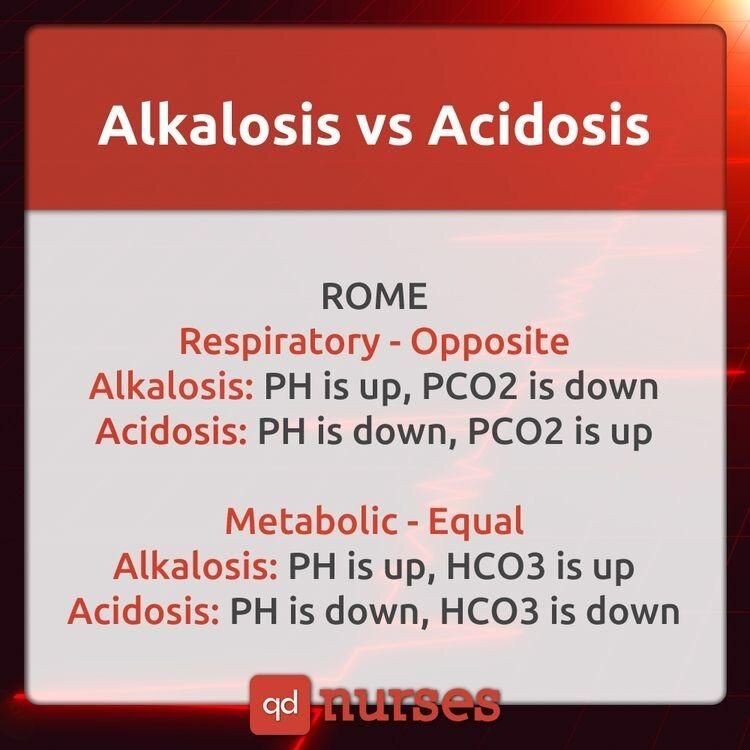
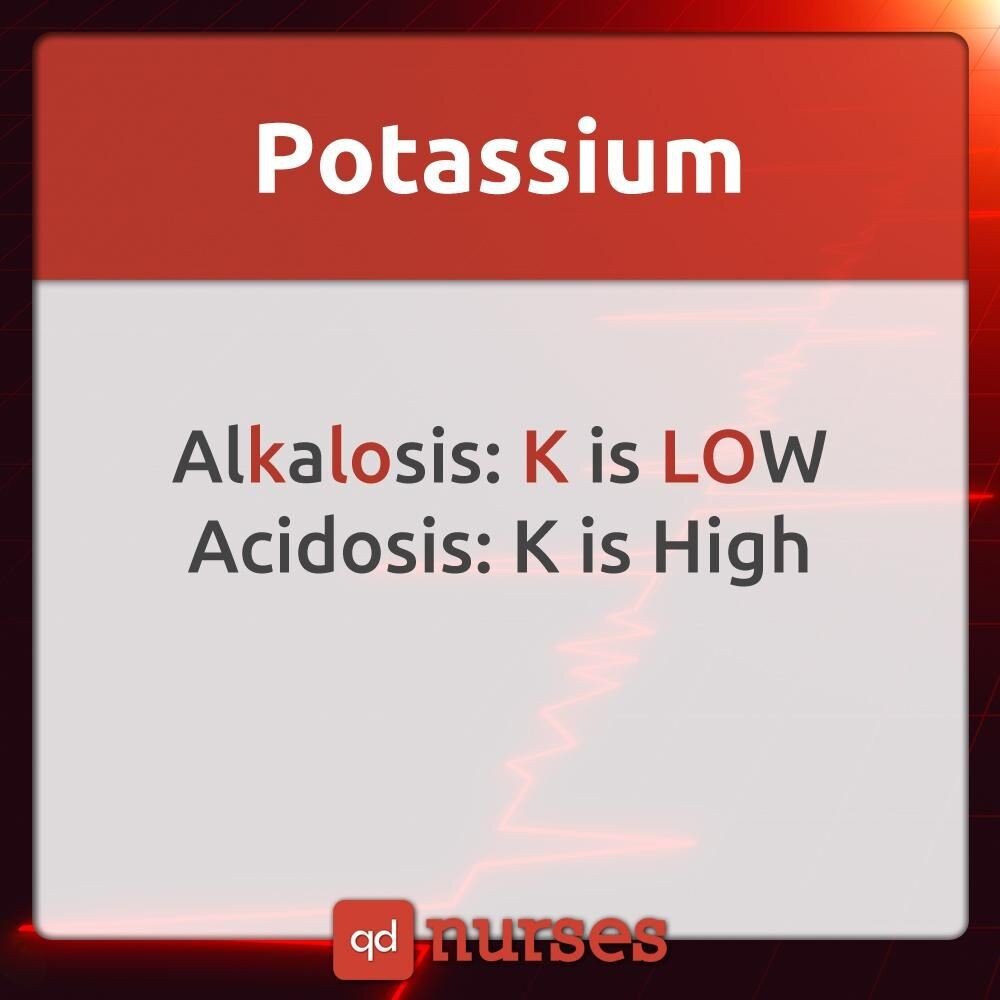
From the a** (diarrhea) = metabolic acidosis From the mouth (vomitus) = metabolic alkalosis
With hyperkalemia– pulse is the first vital sign you check (due to dysrhythmias)
Diet for Iron-Deficiency Anemia

Oysters, clams, scallops are top-10 sources of iron
- Organ meats (red meats), fortified cereals, dark leafy vegetables, egg yolks are also good sources of dietary iron
Iron supplements should be taken with orange juice (Vitamin C) as it facilitates absorption
Documentation should be specific and factual—“Vital Signs Stable” is NOT
acceptable—what are the vital signs?
Herbal Medications
- Potency varies between medications
- Considered dietary supplements
- Not regulated by FDA
- Ma Huang should not be used by patient’s with HTN
- Ginkgo – improves cerebral circulation to treat dementia and memory loss–increases risk of bleeding, increases effects of MAOIs, may reduce effectiveness of insulin—discontinue 2 weeks prior to surgery, may cause seizure with overdose
- Garlic acts as blood thinner
- Black cohosh– used to treat menopause – large doses have been known to cause seizures, visual disturbances, increased sweating, bradycardia
- Feverfew– prevention and treatment of migraines, arthritis, and fever–should not be taken with coumadin, aspirin, NSAIDS, thrombolytics or antiplatelet meds—prolongs bleeding
- Ginseng– improves strength and stamina—prevents and treats cancer and DM–it decreases the effects of anitcoagulants and NSAIDS—contraindicated for women who are pregnant—may increase effectiveness of antidiabetic agents and insulin
- Echinacea– prevents and treats the common cold, stimulates the immune system, promotes wound healing—may reduce the effects of immunosuppressants, may increase serum levels of alprazolam, CCB, and protease inhibitors
- St. John’s Wort– depression and anxiety—may reduce the effects of many medications—theophylline, HIV protease inhibitors, cyclosporine, diltiazem, and nifedipine – should not be taken with other medications
Patients with hearing loss may exhibit suspiciousness of strangers—results from interference with communication
Nausea is a concern/priority following eye surgery—risk of increased IOP
*Patient’s undergoing eye surgery should receive flu shot before—can cause client to sneeze, cough, or blow nose (increasing IOP)
Esophageal speech- (following a total laryngectomy)- swallows air & eructates while forming words
(Organ) Transplant patients- require protective isolation following surgery Most at risk for developing herpes zoster—immunocompromised Cytomegalovirus– common virus –once infected, virus remains in body for life
*Standard precautions are used—eyewear worn with risk of splash
Decreased RBCs/Erythrocytopenia
S/S: fatigue and dyspnea on exertion, pallor, dizziness, malaise, tachycardia
Tetracycline– antibiotic
- Causes photosensitivity – wear sunscreen and hat outdoors
- Should be taken on an empty stomach
- Contraindicated for pregnant women
Sickle Cell Crisis
*Adequate hydration
- Dehydration perpetuates cell sickling—should be at least 200cc/hr
- Do not give cold packs—further decreases blood flow to area and increases sickling
DO NOT GIVE DEMEROL (meperidine) TO PATIENTS WITH SICKLE CELL CRISIS
Phlebitis– reddened area or red streaks at site of catheter
Blanching sign– pressing nail of big toe—indicates circulatory function
Blanching or hyperemia that does not disappear in a short time is a warning sign of pressure ulcers
Severe to panic level of anxiety– patient is unable to process thoughts and feelings for problem solving
Priority when managing a physically assaultive client—restore the client’s self-control and prevent further loss of control
Reward non-attention seeking behaviors by giving client unsolicited attention
Nasogastric Tube
- Patient is nauseated and decreased flow of gastric contents—aspirate and check pH to confirm placement (should be between 0 and 4)
- If irrigation is necessary, use normal saline
- Intermittent feeding
- Check pH of aspirated contents (normal is pH 0-4)
- Use large barreled syringe to aspirate
- Flush with 30 mL of air before aspiration
History of psych patient should include biopsychosocial data; psychosocial and physical status are evaluated along with an assessment of the family system and social support network; evaluation of cognitive ability is important during physiological status assessment
Patients in seclusion should eat at regular time but remain in seclusion for client’s safety
Joint legal custody with divorced parents– consent from either parent is sufficient
Battery is harmful or offensive touching of another person unless court ordered
*For example: Patient refuses medication due to fear that it will poison him—nurse administers medication IM
- Clients have the right to refuse medication even if psychotic
Myelogram
- NPO 4-6 hours
- History of allergies
- Phenothiazines, CNS depressants, and stimulants withheld 48 hours prior
- Table will be moved in various positions during test
- Post- neuro checks q2-4h, oral analgesics for H/A, encourage PO fluids, assess for distended bladder, inspect insertion site
- Water soluble- HOB raised
- Oil soluble- HOB down
Common Signs and Symptoms
- Pulmonary TB– low grade afternoon fever
- Pneumonia– rusty sputum
- Asthma– wheezing on expiration
- Emphysema– barrel chest
- Kawasaki Syndrome– strawberry tongue. Peeling skin on fingers and toes
- Pernicious Anemia– red beefy tongue, pallor, tachycardia
- Down Syndrome– protruding tongue
- Cholera– rice watery stool
- Malaria– stepladder-like fever with chills
- Typhoid– rose spots on abdomen
- Diphtheria– pseudo membrane formation
- Measles– koplik’s spots (clustered white lesions on buccal mucosa)
- Systemic Lupus Erythematous– butterfly rash
- Liver cirrhosis– spider-like varices
- Leprosy– leonine facies (thickened folded facial skin)
- Bulimia– chipmunk face (parotid gland swelling), poor dental status
- Appendicitis– rebound tenderness, psoas sign (pain from flexing the high to the hip); Rovsing’s sign (palpation of LLQ elicits pain in RLQ)
- Meningitis– Kernig’s sign (knee flex and pain on extension), Brudzinski sign (neck flex = lower leg flex/bend), nuchal rigidity, photosensitivity
- Tetany– hypocalcemia (+) Trousseau’s sign/carpopedal spasm, Chvostek sign (facial spasm)
- Tetanus– risus sardonicus
- Pancreatitis– Cullen’s sign (ecchymosis of umbilicus); (+) Grey Turner’s spots
- Pyloric Stenosis– olive-like mass, projectile vomiting
- Patent Ductus Arteriosus– washing machine-like murmur
- Addison’s– bronze-like skin pigmentation (tanned)
- Cushing’s– moon face and buffalo hump
- Grave’s/Hyperthyroidism– exophthalmos (bulging of the eyes)
- Intussusception– sausage shaped mass, Dance sign (empty portion of RLQ), red currant jelly stools
- Multiple Sclerosis– Charcot’s Triad (nystagmus, intention tremor, scanning speech)
- Myasthenia Gravis– descending muscle weakness, ptosis (drooping eyelid)
- Guillain Barre- ascending muscle weakness/paralysis
- DVT– Homan’s sign
- Chicken Pox– vesicular rash (central to distal), dew drop on rose petal
- Angina– crushing stabbing pain, relieved by NTG
- Myocardial Infarction– crushing stabbing pain- radiates to left shoulder, neck, arms, unrelieved by NTG
- Laryngotrachebronchitis– inspiratory stridor
- Transesophageal Fistula– 4 C’s- Coughing, choking, cyanosis, continuous drooling
- Epiglottitis– 3 D’s- drooling, dysphonia, dysphagia (acute emergency)
- Hodgkin’s Lymphoma– painless, progressive enlargement of spleen and lymph tissues, Reedstenberg cells
- Infectious Mono– sore throat, cervical lymph adenopathy, fever, fatigue
- Parkinson’s– pill-rolling tremors
- Cytomegalovirus (CMV) infection– Owl’s eye appearance of cells (huge nucleus in cells)
- Cystic Fibrosis– salty skin, intussuception
- Diabetes Mellitus- polyuria, polydipsia, polyphagia
- DKA- Kussmaul respirations (deep, rapid RR), acetone breath
- Bladder cancer- painless hematuria
- Benign Prostatic Hyperplasia- reduced size and force of urine
- Retinal Detachment- visual floaters, flashes of light, curtain-like shadow vision (emergency situation)
- Glaucoma- painful vision loss, tunnel/gun barrel/halo vision
(peripheral vision loss)
- Cataract- painless vision loss, opacity of the lens, blurring of the vision, change in color vision
- Retinoblastoma- Cat’s eye reflex (grayish discoloration of pupils)—seen in photos
- Pregnancy Induced Hypertension- proteinuria, HTN, edema
- Acromegaly- coarse facial feature
- Duchenne’s Muscular Dystrophy- Gower’s sign (use of hands to push one’s self from the floor)
- GERD- heartburn, Barrett’s esophagus (erosion of the lower portion of the esophageal mucosa)
- Hepatic encephalopathy- flapping tremors (asterixis)
- Hydrocephalus- Bossing sign (prominent forehead)
- Increased ICP- HTN, Bradypnea, Bradycardia (Cushing’s Triad)
- Shock- Hypotension, Tachypnea, Tachycardia
- Meniere’s Disease- vertigo, tinnitus
- Cystitis- burning on urination
- Hypocalcemia- (+) Chvostek and Trousseau’s
- Ulcerative Colitis- recurrent bloody diarrhea
- Lyme’s Disease- Bull’s eye rash
- Buerger’s Disease- intermittent claudication (pain at buttocks or legs from poor circulation resulting in impaired walking)
- Hirschsprung’s Disease (Toxic Megacolon)- ribbon-like stool
STIs
- Herpes Simplex Type II- painful vesicles on genitalia
- Genital Warts- warts 1-2 mm in diameter
- Syphillis- painless chancres
- Chancroid- painful chancres
- Gonorrhea- green, creamy discharges and painful urination
- Chlamydia- milky discharge and painful urination
- Candidiasis- white, cheesy, odorless vaginal discharges
- Trichomoniasis- yellow, itchy, frothy, and foul-smelling vaginal discharges
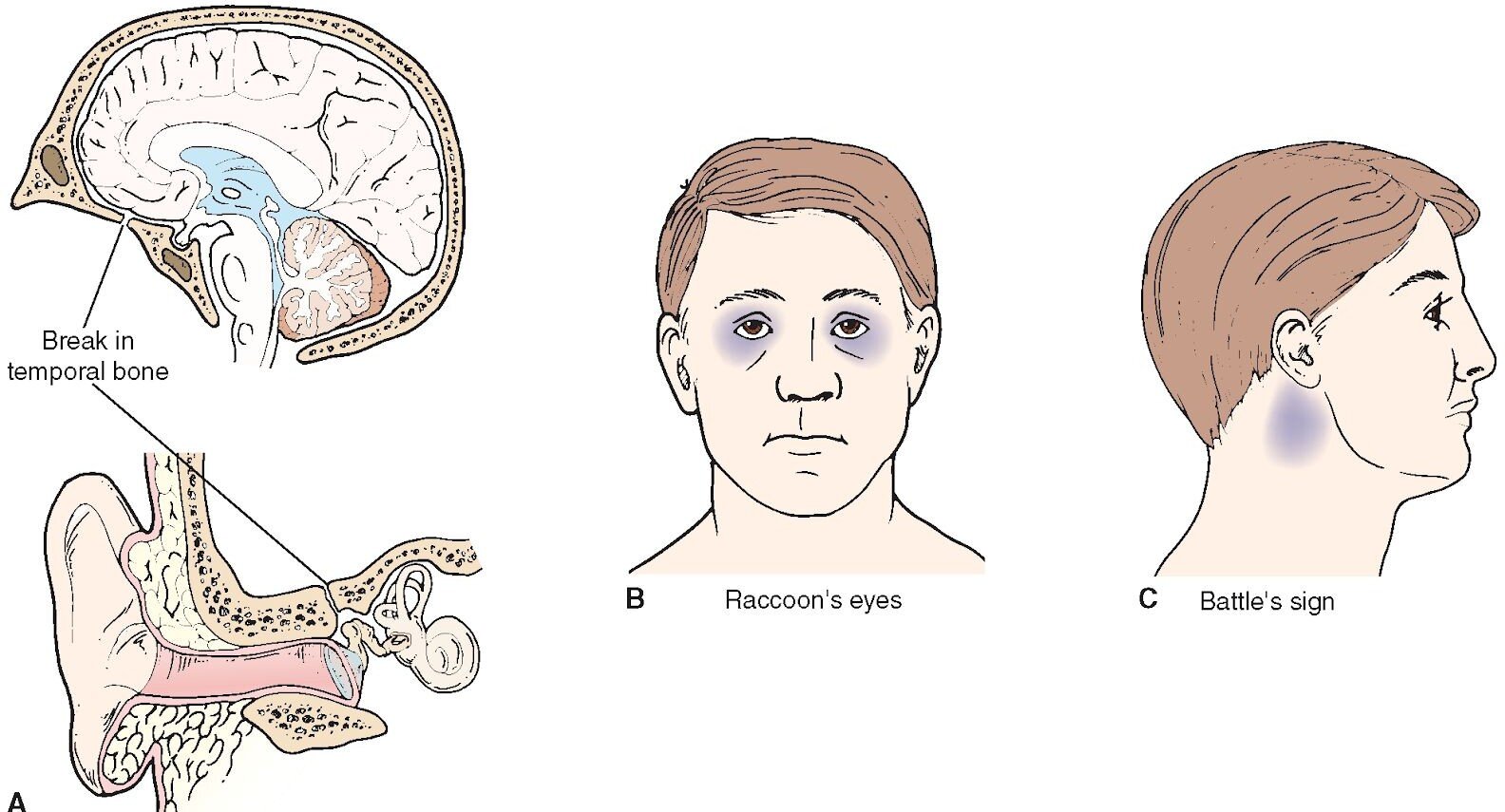 CSF Ottorhea- sign of basilar fracture
CSF Ottorhea- sign of basilar fracture
Battle’s sign and raccoon eyes
NO Nasotracheal suctioning with head injury or skull fracture (increases ICP)
Take iron elixir with juice or water- never with milk!
Therapeutic Drug Levels
Dilantin- 10 to 20
Theophylline- 10 to 20
Acetaminophen – 10 to 20 (do not excess 4000mg in one day) Lithium- 0.4 to 1.4
Digoxin- 0.5 to 2.0
Osteomyelitis is an infectious bone disease- blood cultures and antibiotics—if necessary, surgery to drain abscess
Nephrotic Syndrome– S/S edema (periorbital and generalized), dark, foamy urine (indicating proteinuria), and weight gain due to excessive fluid retention; also HTN
Characterized by massive proteinuria
- Decreased serum albumin
- Patient will receive corticosteroids
*Risk for impaired skin integrity
Glomerulonephritis– cola colored urine, HTN, edema, proteinuria
- V/S q4h
- Daily weights
Common Diets
- Acute Renal Disease– protein-restricted, high-calorie, fluid-controlled, sodium and potassium controlled
- Addison’s Disease– increased sodium, low potassium diet
- ADHD and Bipolar– high-calorie and provide finger foods
- Burns– high protein, high calorie, increase in Vitamin C
- Bowel Surgery– low residue
- Cancer- high-calorie, high-protein
- Celiac Disease- gluten-free diet (No BROW- barley, rye, oat, and wheat)
- Chronic Renal Disease- protein-restricted, low-sodium, fluid-restricted, potassium-restricted, phosphorous-restricted
- Cirrhosis (stable)- normal protein
- Cirrhosis with hepatic insufficiency – restrict protein, fluids, and sodium
- Constipation- high-fiber, increased fluids
- COPD- soft, high-calorie, low-carbohydrate, high-fat, small frequent feedings
- Cystic Fibrosis- increase in fluids, high-sodium
- Diarrhea- liquid, low-fiber, regular, fluid and electrolyte replacement
- Gallbladder disease- low-fat, calorie-restricted, regular
- Gastritis- low fiber, bland diet
- Hepatitis- regular, high-calorie, high-protein
- Hyperlipidemias- fat controlled, calorie-restricted
- HTN, HF, CAD- low-sodium, calorie restricted, fat-controlled
- Kidney Stones- increased fluid intake, calcium-controlled, low oxalate
- Nephrotic Syndrome- sodium-restricted, high-calorie, potassium-restricted
- Obesity, overweight- calorie restricted, high fiber
- Pancreatitis- low fat, regular, small frequent feedings, tube feeding or TPN
- Peptic ulcer- bland diet
- Pernicious Anemia (B12)- increase B12, found in high amounts in shellfish, beef, liver and fish
- Sickle Cell Anemia- increase fluids to maintain hydration since sickling increases when patients become dehydrated
- Spinal Cord Injury- high fiber, low fat (prevent constipation and straining)
- Stoke- mechanical, soft, regular, or tube-feeding
- Underweight- high-calorie, high protein
- Vomiting- fluid and electrolyte replacement An ill child regresses in behavior
Assessing extraocular eye movements– check cranial nerves 3, 4, & 6
DVT
- Goal: promote venous return and decrease in venous pressure
- Bed rest with elevated extremity
Stomas
- Dusky- poor blood supply
- Protruding – prolapsed
- Sharp pain + rigidity- peritonitis
- Mucus in ileal conduit is expected
Tension pneumothorax – trachea shifts to opposite side
Change in color is always a LATE sign
Incentive Spirometer– steps: 1) sit upright 2) exhale 3) insert mouthpiece 4) inhale for 3 seconds and then hold for 10 seconds
MRSA– contact only
VRSA– contact AND airborne (private room, door closed, negative pressure)
Thrombocytopenia- bleeding preacautions
- Soft bristled toothbrush
- No insertion of anything (suppositories, etc.)
- No IM meds as much as possible
Risk of MRSA
- Indwelling foley catheter
- Receiving medication through port, vascular access device, ET tube
- Immunocompromised
Iron deficiency anemia-
- Fe PO- give with vitamin C or on an empty stomach
- Fe via IM- inferon via Ztrak
Pernicious anemia (B12)- red beefy tongue, will take B12 for life
Meniere’s Disease– restrict sodium, lay on affected ear when in bed, diuretics to decrease endolymph in cochlea
Triad: vertigo, tinnitus, N/V
Dehiscence of abdominal wound with organ evisceration—elevate HOB to 15 degrees → reduces stress on suture line
*May also be placed supine with hips/knees bent
Gastric ulcer pain– occurs 30 min to 90 min after eating, not at night and does not go away with food
Pediatric Tips
- Intraosseous infusion– in pediatric life-threatening emergencies, when IV access cannot be obtained, an osseous (bone) needle is hand-drilled into a bone (usually tibia), where crystalloids, colloids, blood products and drugs can be administered into the marrow—it is temporary- when venous access is achieved it is d/c’d
- Only medication that CANNOT be administered IO is isoproterenol (a beta agonist)
- With glomerulonephritis– consider blood pressure to be the most important assessment paremeter
- Dietary restrictions you can expect- fluids, protein, sodium, and potassium
- In congenital cardiac defects that result in hypoxia– body attempts to compensate for with an influx in immature RBCs—labs that support this: increase Hct, Hgb, and RBC count
- There is an association between low-set ears and renal anomalies- develop around the same time (they are also similar in shape)—if a newborn has low-set ears, this warrants renal function tests
- School-age kids (5 and up) are old enough and should have an explanation of what will happen a week before surgery (such as tonsillectomy)
- First sign of pyloric stenosis in a baby is mild vomiting that progresses to projectile vomiting – later you may be able to palpate a mass, the baby will seem hungry often, and may spit up after feedings
- Kawasaki’s Disease– causes heart problems—coronary artery aneurysms due to inflammation of blood vessels
- A child with a VP shunt will have a small upper-abdominal incision—this is where the shunt is guided into abdominal cavity-watch for: abdominal distention → fluid from the ventricles (in brain) will be redirected to abdomen; watch for signs of increasing ICP→ irritability, bulging fontanels, high-pitched cry in an infant; lack of appetite and headache in a toddler
- Bed position after shunt placement- FLAT→ do not want the fluid to shift too rapidly (if signs of increasing ICP are present—elevated HOB 15-30 degrees)
- Mechanical ventilation can cause bronchopulmonary dysplasia—other causes: infection, pneumonia, or conditions that result in inflammation and scarring
It is essential to maintain nasal patency in a child < 1 year because they are nose breathers
- A child should not be drinking too much milk- it reduces the intake of other essential nutrients—especially iron (could lead to anemia)
If you can remove the white patches from the mouth of a baby it is formula- if you can’t it is candidiasis \
- MMR and Varicella immunizations come later (15 months)- letters are later in alphabet
- Undescended testis or cryptorchidism is a known risk factor for testicular cancer- start teaching boys about self testicular exams around 12
– most cases of testicular cancer occur in adolescence
- Stranger anxiety is greatest between 7-9 months
- Separation anxiety starts around 4-8 months, peaks in toddlerhood (1-3 years)
- For a child exhibiting separation anxiety—offer favorite blanket or toy, talk to infant when leaving room, allow to hear parent’s voice on telephone
- Children frequently set their own pace for development
- Mock run through surgery is a great way to prepare a 5 year old
Always report suspected cases of child abuse
- Eardrop administration for kids <3 years- pinna down and back
- With omphalocele and gastroschisis (herniation of abdominal contents) dress with loose saline dressing with plastic wrap (non-adherent)—monitor temperature (lose heat quickly)
- After hydrocele repair, provide cold therapy (ice) and scrotal support
- NO phenylalanine with positive PKU (no meat, no dairy, no aspartame/artificial sweetener)
- Lofenalac formula
- The biggest concern with cold stress and the newborn is respiratory distress
Normal RR for newborn: 30- 60
- Toddlers need to express autonomy (independence)
- Theories about bed-wetting relate it to immature bladder and deep sleep patterns—most children stop bed-wetting by the time they start school
- Average circumference of the head ranges from 32-36 cm (increase in size may indicate hydrocephalus or increased ICP)
- Between ages 6 and 12, children grow about 2 inches per year and gain 4.5-6.5 lbs/year
- The incidence of once-common infectious disease such as measles, chickenpox, and mumps has been most effectively reduced by the immunization of all school-age children
- Exposure to chemicals in the eyes→ irrigate for 20 minutes → another adult, if present, should call the Poison Control Center and 911
- Children have proportionately larger heads that predispose them to head injuries
- Hypoxemia is more likely in children because of their higher oxygen demand
- Liver and spleen injuries are more likely because the thoracic cage of children offers less protection
- Hypothermia is more likely because of children’s thinner skin and proportionately larger body surface area
- Kawasaki disease is the only exception for children taking aspirin
- Important for children’s to receive immunizations
- National guidelines indicate that medication dosing for pediatric patients should be based on the child’s weight (kg)
- Some sources say that BSA is the most accurate method for dosing in children

Safety- Pediatrics Infant
- Aspiration and suffocation– chop food in fine pieces, appropriate toys, no plastic bags and balloons (latex balloons are the leading cause of pediatric choking deaths)
- Bodily harm – keep sharp objects out of reach, keep infants away from heavy objects they can pull down on themselves, do not leave unattended with animals, monitor for shaken baby syndrome
- Burns– check temperature of water, working smoke detectors in home, handles of pots and pans should be turned to back of stoves, sunscreen should be used, electrical outlets should be covered, clothing should be flame retardant
o Water heater should be set to no greater than 120 degrees
- Drowning– never leave infant unattended near water such as tubs, toilets, and swimming areas
- Falls- never leave unattended, place safety gates on stairs
- Poisoning– lock or remove all toxic substances, mediations should be stored in safety bottles and locked in cupboard, never refer to medication as candy, poison control number handy
- Motor Vehicle Injuries– placed in approved rear-facing car seats in the backseat- preferably in the middle (away from airbags and side impact)—rear facing car seats until 2 years of age and they exceed the manufacturer’s recommended weight (usually 20lbs)
Toddler
- Aspiration and suffocation- avoid common causes of choking- hot dogs, nuts, grapes, peanut butter, raw carrots, tough meat, popcorn, no balloons or plastic bags, no pillows in cribs, no drawstrings on clothing
- Bodily harm- firearms kept in locked boxes, stranger safety
- Burns- (same as above)
- Drowning– (same as above), taught to swim
- Falls– (same as above)
- Motor Vehicle Injuries– airbags near the child should be inactivated, forward-facing until they exceed manufacturer’s weight limit, backseat, booster seat after they have exceeded weight for forward-facing carseat
- Poisoning– avoid exposure to lead paint, safety locks
Preschooler (3 to 6)
- Same as above
- *Encourage safety equipment (helmet)
School-Age Child (6 to 12)
- Bodily harm– firearms should be kept in locked boxes, no trampolines, safe areas for play, stranger safety, wear helmets
- Burns– teach fire safety and potential burn hazards
- Drowning- teach to swim
- Motor vehicle injuries– younger than 13 should be in back seat, airbags inactivated
- Substance abuse-community resources, family involvement
Adolescent (12 to 20)
- Three leading causes of death in adolescents are homicide, suicide, and
motor vehicle accidents
Potassium is lost when a client is taking a thiazide diuretic – monitor K, increase dietary K
- Should not be taken at night- prevent nocturia
Hypokalemia
- ECG changes- ST segment depression, inverted T waves, prominent U waves—may also experience heart block
- Lethargy and muscle weakness
Neck veins are normally distended when patient is supine—veins flatten when sitting
*Decreased plasma volume→ flattened neck veins when supine Nurse is not required to explain delegated assignments
Migraines
- Fatigue is a trigger
Validation of a nurse having a substance abuse problem does not override quality client care! Take care of the patient first!
Hemorrhagic shock– PRIORITY→ identify source of bleeding and apply direct pressure
ECT
- NPO after midnight
- General anesthesia
- Memory loss is an expected outcome
Patients with severe immunodeficiency may be unable to produce an immune response—as a result, a negative TB skin result does not completely rule out a TB diagnosis for this patient → chest x-ray and sputum culture will be ordered.
Patients taking immunosuppressive medications are at an increased risk for development of cancer!
Cultural Considerations
- African Americans– many believe that illness is caused by supernatural causes and seek advice and remedies from faith healers; family oriented; higher incidence of HTN and obesity; high incidence of lactose intolerance
- Arab Americans– may remain silent about health problems such as STIs, substance abuse and mental illness; if Muslim- many avoid pork and alcohol
- Asian Americans– may value ability to endure pain and grief with silent stoicism; hot/cold, yin/yang, sodium intake is generally high; may prefer to maintain a comfortable distance; may believe prolonged eye contact is rude and invasion of privacy
- Latino Americans– may view illness as sign of weakness, punishment for evil doing; family members are typically involved in all aspects of decision making such as terminal illness
- Native Americans– may turn to a medicine man to determine the true cause of an illness, may value the ability to endure pain or grief with silent stoicism, diet may be deficient in Vitamin D and calcium due to lactose intolerance, obesity and diabetes are major concerns
- Western Culture– may value technology almost exclusively in the struggle to conquer diseases; health is understood to be the absence, minimization or control of disease process
Delegation Tips
DO NOT delegate what you can EAT E- evaluate (nursing judgment)
A-assess (nursing judgment)
T- teach
- Delegate sterile skills to RN or LPN
- Where non-skilled care is required, delegate stable client to nursing assistant
- Assign the most critical client to the RN
- Clients who are being discharged should have the final assessments and teaching done by the RN
- A new nurse should receive stable patients who require routine care (same applies to nurses that are transferred to different units for the day)
- The LPN can monitor clients with IV therapy, insert urinary catheters, feeding tubes, and apply restraints
- LPN/LVN cannot handle blood
- LPN/LVN are given stable patients – can perform sterile procedures on stable patients
- Experienced LPNs can use observation of patients to gather data regarding how well they perform interventions that have already been taught (including checking for therapeutic response/adverse effects of medications)
- Assisting with ADLs is appropriate for assistive personnel (record I/O too) Always check for allergies before administering antibiotics (especially penicillin) – or any medication for that matter!
Neutropenic precautions- no live vaccines, no fresh fruits, no flowers, no sick visitors, no milk
- Any temperature elevation in a neutropenic patient may indicate the presence of a life-threatening infection
- Patients who are neutropenic should be place in a positive-airflow room
In the event of a fire- RACE→ (R) Remove the patient (A) Activate the alarm (C) Contain the fire by closing the door (E) Extinguish the fire if it can be done safely
Informed consent– patient should know whether other treatment options are available and should understand what will occur during the preoperative, intraoperative, and postoperative phases; the risks involved, possible complications—always allow patient to ask questions!
Veracity is truth and is an essential component to a therapeutic relationship between a healthcare provider and patient
Beneficence is the action that is done to benefit others
Nonmaleficence is the duty to do no harm
Projection is the unconscious assigning of a thought, feeling, or action to someone or something else
Sublimation is the channeling of unacceptable impulse into socially acceptable behavior
Repression is an unconscious defense mechanism whereby unacceptable or painful thoughts, impulses, memories, or feelings are pushed from the consciousness or forgotten
People with obsessive-compulsive disorder realize that their behavior is unreasonable, but are powerless to control it
Hypervigilance and déjà vu are signs of PTSD
Health Screening for Cancer
CAUTION
C- change in bowel or bladder habits
A- a sore that does not heal
U- unusual bleeding or discharge
T- thickening or lump in breast or elsewhere
I- indigestion or difficulty swallowing O- obvious change in a wart or mole N- nagging cough or hoarseness
Common sites for metastasis– liver, brain, lung, bone, lymph
When a cancer patient is receiving radiation– main concern is preventing infection because radiation causes leukopenia
Radioactive Iodine– want to flush it out of body → increase fluid intake for 2 days (3-4 liters unless otherwise contraindicated)—flush the toilet twice after using
*Limit contact with patient to 30 min/day
NO PREGNANT VISITORS/NURSES and no kids
The main hypersensitivity reaction seen with antiplatelet drugs is bronchospasm (anaphylaxis)
- Ex: clopidogrel, aspirin
Do not fall for the “reestablishing a normal bowel pattern” as a priority with small bowel obstruction—the patient can’t take in oral fluids, “maintaining fluid balance” comes first!
Basophils release histamine during an allergic reaction
Other than to initially test tolerance- G tube and J tube feedings are usually given as continuous feedings
Tamoxifen (chemotherapy agent) can cause visual changes—can be irreversible—assess visual acuity throughout treatment
You should ask every new admission if he/she has an advance directive
Succinylcholine Chloride (Anectine)- used for short-term neuromuscular blocking agents for procedures like intubation and ECT
Typical adverse reactions to oral hypoglycemic– rash and photosensitivity
Hypotension may alter the accuracy of O2 sats
An antacid should be given to a mechanically ventilated patient with NG tube if the pH of the aspirate is <5.0—aspirate should be checked at least q12h
Ambient air (room air) contains 21% oxygen
Normal PCWP (pulmonary capillary wedge pressure) is 8-13 → readings of 18-20 are considered high
High potassium (hyperkalemia) is expected with carbon dioxide narcosis (hydrogen floods the cell, forcing potassium out)- carbon dioxide narcosis causes increased ICP
An NG Tube can be irrigated with cola and should be taught to the family when a client is going home with the tube
If your normally lucid patient starts seeing bugs, check respiratory status FIRST—the first sign of hypoxia is restlessness, followed by agitation (continues to decline from there) → leads to delirium and hallucinations, and eventually coma!
- Check O2 stat
- ABGs if possible
Status epilepticus – most important assessment is level of consciousness
Pneumonia may manifest itself as mental confusion due to hypoxia Can’t cough → ineffective airway clearance
If a patient has low Hgb/Hct—should be evaluated for signs of bleeding (dark/black stools)
A patient with liver cirrhosis and edema may ambulate, then sit with legs elevated to try to mobilize the edema
Safety over nutrition in a severely depressed patient
Depression can manifest itself in somatic ways- such as psychomotor retardation, GI complaints and pain
Prolonged hypoxemia is a likely cause of cardiac arrest in a child
Coarctation of the aorta causes increased blood flow and bounding pulses in the arms
Newly diagnosed HTN- assess BP in both arms
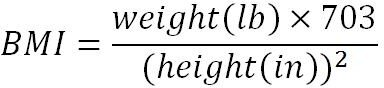
Place a wheelchair parallel to the bed on the strong side Gonorrhea is a reportable disease!
Stairway to Heaven (Crutches)
- The good go to heaven- good leg goes up the stairs first with crutches (crutches move with the affected leg)
- The bad to to hell (down)- bad leg goes down the stairs first (crutches move with the affected leg)
Vasopressin– “press in” → vasoconstriction (used when patient is hypotensive)
Burning sensation in the mouth and brassy taste are adverse reactions to Lugol Solution (iodine) – used in treatment of hyperthyroidism
Nonfat milk reduces reflux by increasing lower esophageal sphincter pressure
When the oxygen flow rate is higher than 4L/min, the mucous membranes can be dried out- the best treatment is to add humidification to the oxygen delivery system (applying water-soluble jelly to the nares can also help decrease mucosal irritation)
A nonrebreather mask can delivery nearly 100% oxygen—when the patient’s oxygenation status does not improve adequately in response to delivery of oxygen at this high concentration, refractory hypoxemia is present—usually at this stage, the patient is working very hard to breathe and may go into respiratory arrest unless healthcare providers intervene by providing intubation and mechanical ventilation
The endotracheal tube should be marked at the level where it touches the incisor tooth or nares—this mark is used to verify that the tube has not shifted
Infections are always a threat for the patient receiving mechanical ventilation—elevated temperature is cause for concern
Confusion in a patient taking enoxaparin (Lovenox) could indicate intracerebral bleeding!
Removing large quantities of fluid from the pleural space can cause fluid to shift from the circulation into the pleural space, causing hypotension and tachycardia—may need IV fluids to correct this
Low sodium diet is 2g or less
Persistent and irritating cough (dry cough caused by accumulation of bradykinin) is a possible adverse effect of ACE-inhibitors (enalapril) and is a common reason for changing to another medication category such as ARBs
The goal when treating HTN with medication is reduction of blood pressure to under 140/90
Because continuous chest pain lasting more than 12 hours indicates that reversible myocardial injury has progressed to irreversible myocardial necrosis, fibrinolytic drugs (TPA) are not recommended for clients with chest pain that has lasted for more than 12 hours
The goal in pain management for the client with an acute MI is to completely eliminate the pain. Even pain rated at a level of 1 out of 10 should be treated with additional morphine sulfate
Hyperkalemia is a common adverse effect of both ACE inhibitors and potassium-sparing diuretics
Proton pump inhibitors (omeprazole) affect the metabolism of clopidogrel and decrease its effectiveness
The most common complication after coronary arteriography is hemorrhage—earliest indication of hemorrhage is an increase in heart rate
PVCs occurring in the setting of acute MI can lead to ventricular tachycardia and/or v-fib (cardiac arrest), so rapid treatment is necessary
Anticoagulant medications are high-alert meds and require special safeguards- such as double-checking medication by two nurses before administration
B-type natriuretic peptide levels increase in clients with poor left ventricular function and symptomatic heart failure and can be used to differentiate HF from other causes of dyspnea and fatigue (such as pneumonia)
A patient with thrombocytopenia (low PLT count) should not take aspirin routinely—aspirin decreases platelet aggregation
When a hemophiliac patient is at high risk for bleeding, the priority intervention is to maximize the availability of clotting factors (administer Factor VII)
Hemophilia is x-linked – mother passes to son
Joint pain in hemophilia indicates bleeding—treatment includes factor VII and RICE
Bence Jones proteins in the urine indicate multiple myeloma
Increased risk of infection after splenectomy—monitor for elevation of temperature
Fatal hyperkalemia may be caused by tumor lysis syndrome, a potentially serious consequence of chemotherapy in acute leukemia
A non-tender lump or swelling near lymph nodes may indicate that the patient has developed lymphoma (possible adverse effect of immunosuppressive therapy
A newly-admitted patient needs to be assessed as soon as possible—if all patients are stable, the new admission takes priority because plan of care needs to be completed
Order of a newborn bath:
- Place on warm surface
- Cleanse eyes
- Cleanse face
- Cleanse body with warm water
- Wrap infant in pre-warmed blanket
- Shampoo head/hair
If TPN is not ready when it is due, D10W or D20W should be administered
- Always check the order before administering TPN—generally each bag is individually prepared by the pharmacist
- Solution should not be cloudy or turbid
- Prime the tubing and thread the pump
- To prevent infection, scrub the hub and use aseptic technique when inserting the connector into the injection cap and connecting the tubing to the central line
- Set the pump at the prescribed rate
Probiotic therapy- live microorganisms similar to those found in GI track—when colonized they enhance the immune response and stabilize the mucosal barrier in the digestive track
- Patients who may benefit:
- Antibiotic associated diarrhea
- IBS
- Lactose intolerance
(+) nitrite in urine is indication of UTI
- Other signs: elevated WBC count, elevated temp, confusion in elderly, burning with urination
- minute hand scrub is particular to the newborn nursery area and included in medical asepsis
Medical asepsis = clean technique
Two identifiers must be used when administering medication
-
- Name on bracelet
- Photo
- Bar code system
- Asking patient to state name
“Time Out”
-
- Called before the initiation of any surgical procedure
- Patient can be involved
Goals
-
- Correctly identify the patient
- Correctly identify the site and side
- Verify that OR team agrees on procedure
Oculogyric crisis– eyes locked upward (acute dystonic reaction from antipsychotic medications)—contact physician- anticipate administration of anticholinergic medication- benztropine (cogentin)
Talipes equinovarus– club foot
The priority for migraine headache is pain management
A client with a seizure disorder should not take OTC medications without consulting with the health care provider first
First priority for the client with a spinal cord injury is assessing
respiratory patterns and ensuring an adequate airway
Priority intervention for a client with Guillain Barre Syndrome is maintaining adequate respiratory function—clients with Guillain Barre are at risk for respiratory failure, which requires urgent intervention
Clients with right cerebral hemisphere stoke often manifest neglect syndrome—lean to the left, when asked, respond that they believe they are sitting up straight—often neglect the left side of their bodies and ignore food on the left side of their food trays
Bacterial meningitis is a medical emergency- antibiotics are the priority medication (cultures and specimens should be drawn before)
Priority action during a generalized tonic-clonic seizure is to protect the airway by turning the client to one side—oxygen is used in postictal phase
Exophthalmos– instill artificial tears (hyperthyroidism- Graves) Bulge test confirms presence of fluid in knee- leg should be extended Side rails should always be elevated for disoriented patients
Bismuth subsalicylate absorbs PO meds and should be administered separately
Normal CVP– 3-12 mmHg (cm of water)
Early signs of hepatic encephalopathy
- Impaired thought process
- Insomnia and sleep disturbances
- Tremors
Sengstaken-Blakemore tube– have scissors at bedside (airway obstruction→ cut balloon with scissors)
Nurse is obligated to share client information with personnel directly involved in care
Bowel perforation requires emergency surgery (result of increased intraluminal pressure)—intestinal contents are released into peritoneum leading to peritonitis
Heat in cast is a sign of pressure, which can indication poor circulation! Requires fast assessment!
Hypotonic (0.45% NS) shifts fluid into intracellular space
Radium implant– strict bed rest (so no, they cannot use a bedside commode) Cyclophosphamide – will likely cause alopecia 4-5 weeks after starting Bell’s Palsy– use artificial tears (4x/day)
Cocaine Abuse S/S
- Insomnia
- Rhinorrhea
- Tachycardia
- Euphoria
*Cocaine is a stimulant
Low titer means risk for developing disease
Breathing slowly will enhance relaxation of abdominal muscles
Shingles– able to care for non-high risk clients—cover lesions
- Should not care for pregnant women, premature infants, immunocompromised
Parenteral Nutrition (PN)- monitor serum glucose and electrolytes
- Most common complication involves fluid and electrolytes No Beta-Blockers with COPD
No lidocaine with heart blocks→ diminishes existing ventricular response
Causes of tinnitus
- Aspirin
- Diuretics
- Neurological conditions
- Loud noises
- Impacted earwax or foreign bodies in the ear
- Ear infections
A bulging red or blue tympanic membrane is a possible sign of otitis media or perforation
Vertigo without hearing loss should be further assessed for nonvestibular causes, such as cardiovascular or metabolic problems!
Stapedectomy (surgical procedure of the middle ear; used for hearing loss related to otosclerosis)
- Heavy lifting should be avoided for at least 3 weeks after the procedure
- Water in the ear, and air travel should be avoided for at least 1 week
- Coughing and sneezing should be performed with the mouth open to prevent increase pressure in the ear
Ear Irrigation
- Use an otoscope to assess the ear first
- Fill syringe with warm fluid
- Angle the syringe to allow the fluid to flow along the side of the ear canal, not directly at the eardrum
- Flush with continuous pressure, rather than a pumping action
- You should see fluid return with cerumen
- If not, wait at least 10 minutes and repeat
- Tipping the head allows gravity drainage of fluid left in the ear canal
Basilar invagination (platybasia) causes brainstem manifestations- can be life threatening
4 C’s of Communication
- Clear
- Concise
- Correct
- Complete
*Ensures the staff understands what is being said
Postoperative pain and numbness occur for a longer period of time with
endoscopic carpal tunnel release than with an open procedure.
- Hand movements, including heavy lifting, may be restricted for 4-6 weeks after surgery
- Patients experience discomfort for weeks to months
- Surgery is not always a cure
- In some cases CTS may recur months to years after surgery
Fat embolism syndrome is a serious complication that often results from fractures of long bones—its earliest manifestation is altered mental status caused by a low arterial oxygen level
The goal of bowel training is to establish a pattern that mimics normal defecation, and many people have the urge to defecate after a meal
Refeeding syndrome occurs when aggressive and rapid feeding results in fluid retention and heart failure—monitor for signs of fluid volume overload
Substance abuse may exclude a person from the transplant list
The presence of glucose in the nasal drainage indicates the fluid is CSF (cerebrospinal fluid) and suggests a CSF leak
Vitiligo, or patchy areas of pigment loss with increased pigmentation at the edges, is seen with primary hypofunction of the adrenal glands and is caused by autoimmune destruction of melanocytes in the skin
Silver scaling on skin is associated with psoriasis
Wounds should be debrided before obtaining wound specimen for culturing
Isotretinoin – oral medication used for acne—has high incidence of birth defects—important to stop using medication at least a month before attempting to become pregnant
Wheals (on the skin) are frequently associated with allergic reactions—asking the patient about exposure to new medications is the most appropriate question
Chemical/toxic exposure to skin→ priority is to remove the chemical from contact with the skin to prevent ongoing damage
Prostate disease increases the risk of UTIs in men because of urinary retention A cystoscopy is needed to accurately diagnose interstitial cystitis
A patient with urge incontinence can be taught to control the bladder as long as the patient is alert, aware, and able to resist the urge to urinate by starting a schedule for voiding, then increasing intervals between voids
Women should avoid irritating substances such as bubble baths, nylon underwear, and scented toilet paper to prevent UTIs
Bruising is expected post-lithotripsy and can be quite extensive
A patient with only one kidney should avoid all contact sports and high-risk activities to protect the remaining kidney from injury and preserve kidney function
During the oliguric phase of acute kidney failure, a patient’s urine output is greatly reduced. Fluid boluses and diuretics do not work well. This phase usually lasts from 8-15 days
Patients with acute kidney failure usually go through a diuretic phase 2 to 6 weeks after the oliguric phase—the diuresis can result in an output of up to 10L/day of dilute urine→ during this time it is important to monitor for electrolyte and fluid imbalances
MAP = [ (2 x diastolic) + systolic ] divided by 3
A palpable bladder and restlessness are indicators of urinary retention, which requires action to empty the bladder (such as catheterization)
Benign prostatic hyperplasia (BPH)
- Client will have trouble starting a urinary stream
- Elevated level of prostate-specific antigen
Irregularly shaped and nontender lumps are consistent with a diagnosis of
breast cancer
Transurethral Resection of the Prostate (TURP)
- Bladder spasms may indicate that clots are obstructing the catheter, which would indicate the need for irrigation of the catheter with 30 to 50 mL of NS using a piston syringe (irrigation would be first action)
- Hemorrhage is a major complication following a TURP—signs would be catheter draining deep red blood
Tamulosin– used to treat BPH — monitor for orthostatic hypotension
- Improves symptoms by relaxing the muscles in the prostate and bladder neck—making it easier to urinate
- Force of urinary stream may increase
Testicular Torsion
- Scrotal swelling and severe pain—likely not relieved or decreased by elevation of the scrotum
- Emergency situation that requires immediate assessment and intervention because it can lead to testicular ischemia and necrosis within a few others
Sildenafil (Viagara)- potent vasodilator used in the treatment of erectile dysfunction
- Has caused cardiac arrest in clients who were also taking nitrates such as nitroglycerin
After an A&P repair (vaginal wall repair/anterior and posterior), it is essential that the bladder be empty to avoid putting pressure on the suture lines
- Abdominal firmness and tenderness indicate that the bladder is distended—requires catheterization
Rapid Response Team (RRT)
- Role of RRT is the immediate assessment and stabilization of a client
First-degree relatives of patients with the BRCA gene should be screened annually with both mammography and MRI
Severe spontaneous hemorrhage is not expected until the platelet count drops below 20,000 mm3
Frequent swallowing following T&A may indicate bleeding
Tracheal deviation suggests tension pneumothorax– priority situation→ requires chest tube
Synthetic surfactant improves respiratory status and decreases the incidence of pneumothorax in premature infants with respiratory distress syndrome (RDS)
Crackles throughout both lungs indicate that a child has severe left ventricular failure as a complication of endocarditis
Decreased responsiveness in a patient with a clotting disorder may indicate intracerebral bleeding—priority situation
Chlamydia is the most prevalent STI in the US—screening is strongly recommended for all sexually active females 25 years or younger
Iron is a toxic substance that can lead to massive hemorrhage, coma, shock, and hepatic failure—deferoxamine is an antidote that can be used for severe cases of iron poisoning
Triage requires at least one experienced RN
Primary survey for a trauma patient arriving to ED includes a brief neurologic assessment to determine level of consciousness and pupil reaction
Secondary survey includes measuring vital signs, assessing the abdomen, and checking pulse oximetry readings
Heat stroke is a medical emergency that increases the risk for brain damage
You respond to a call for help from the ED waiting room—an elderly client is lying on the floor….
- Establish responsiveness first (the client may have fallen and sustained a minor injury)
- If the client is unresponsive, get help and activate the code team
- Performing the chin lift or jaw thrust maneuver opens the airway
- The nurse is then responsible for starting CPR
o CPR should not be interrupted until the client recovers or it is determined that all heroic efforts have been exhausted
- A crash cart should be at the site when the code team arrives—however, basic CPR can be effectively performed until the team is present
Pulsating mass in abdomen indicates abdominal aneurysm—concern is rupture
A person who experienced a threat to his or her own life is at the greatest risk for psychiatric problems following a disaster incident (such as PTSD)
Appropriate in Disaster Triage
- Check airway, breathing, circulation
- Assess the level of consciousness
- Visually inspect for gross deformities, bleeding, and obvious injuries
- Note color, presence of moisture, and temperature of the skin
- Check vital signs, including pulse and respirations
Patients with conversion disorders are experiencing symptoms, even though there is no identifiable organic causes→ therefore they should be assisted in learning ways to cope and live with the disability
Family history of completed suicide is a risk factor for an individual committing suicide
Before someone enters an alcohol rehabilitation program, there should be a medically-supervised detoxification
When delegating psychiatric patients to new RNs, try to avoid assigning a psychotic patient – they can be very threatening to new RNs
Restraints must be tied to a stationary portion of the bed using quick-release knots→ distal pulses should be checked
- Restraints are rarely a planned event
Take time for yourself—a mind that is fried, is not a good use of time!